胃癌是临床最常见的消化道癌,其发病率和 病死率逐年上升,2012年的全球肿瘤发病率报告中提到,目前50%的新发胃癌患者集中在东南亚国家,主要在中国,已经严重威胁到人们的生命健康[1-2]。目前,临床上外科治疗胃癌的方法主要是通过胃根治性切除来治疗,该手术主要有开放性和腹腔镜两种手术方式。开放性手术虽然效果好,手术时间短,但创伤大,术后恢复时间长以至于患者依从性较差,而腹腔镜手术因难度较大,对操作者要求高、手术时间较长,但创伤小、术后住院时间短。因此,两种手术方式各有利弊,如何正确认识两种手术方式的优缺点,是目前摆在大部分外科医生面前的一道难题。因此,本研究中心通过比较完全腹腔镜与开放性全胃切除术中情况和术后并发症的差异,探讨两种手术方式的各自的可行性,并通过对并发症的影响因素的分析,进一步了解加强对术后并发症的控制。
1 资料与方法
1.1 一般资料
收集2014年1月—2017年1月由本院普外科病区同一治疗组的医师施行的完全腹腔镜下胃癌根治性全切术患者150例(腔镜组),行开腹手术患者180例(开腹组),利用两组患者的临床围手术期各阶段的资料进行回顾性分析,纳入标准:⑴ 术前胃癌病理诊断明确;⑵ 术前影像学资料齐全并提示无其他脏器及远处转移;⑶ 术后病理学诊断为R0切除。剔除标准:⑴ 肿瘤种植及远处转移者;⑵ 行姑息性手术者;⑶ 病理学诊断资料不全者。最终将330例胃癌行外科手术的患者纳入本次研究中,其中男191例,女139例;年龄35~86(57.6±11.3)岁。对腹腔镜组和开放组患者的一般情况的资料进行统计学分析,差异无统计学意义(均P>0.05),具有可比性(表1)。
表1 两组患者的一般情况比较
Table 1 Comparison of the general data between the two groups of patients

1.2 手术方法
1.2.1 开放组手术 患者取平卧位,予以气管插管全麻,麻醉平稳后,消毒铺巾并贴膜,予患者上腹正中绕脐15~20 cm切口,严格遵循胃癌根治术要求开展手术,根据实际情况实施全胃切除、肠道吻合,采用胃十二指肠端-侧吻合,并实施淋巴结清扫 。
1.2.2 腔镜组手术 取患者平卧位,建立气腹及套管穿刺,全身麻醉,麻醉满意后消毒铺巾。取患者脐上弧形小切口,经小切口以巾钳提起腹壁皮肤,建立气腹,维持气腹压力15 mmHg(1 mmHg=0.133 kPa)。经患者脐上小切口采用12 mm套管穿刺,置入腹腔镜,于腹腔镜定位下经左右上腹分别采用5 mm套管各穿刺牵引孔1个。于患者脐水平左侧5 cm处10 mm套管穿刺主操作孔,于患者脐水平右侧相对位置以5 m套管穿刺主操作孔。施行胃大部切除及区域淋巴结清扫。最后经肚上操作孔做一小切口,切口保护套保护切口,取出标本送检。
1.3 观察指标
比较腔镜组和开放组的手术时间、术中出血量、术后胃肠功能恢复时间、术后住院时间、清扫淋巴结数目及术后各种并发症发生情况。
1.4 统计学处理
利用SPSS l9.0软件实现对本两组数据的对比分析,计量资料比较采用t检验,计数资料比较采用χ2检验。P<0.05为差异具有统计学意义。
2 结 果
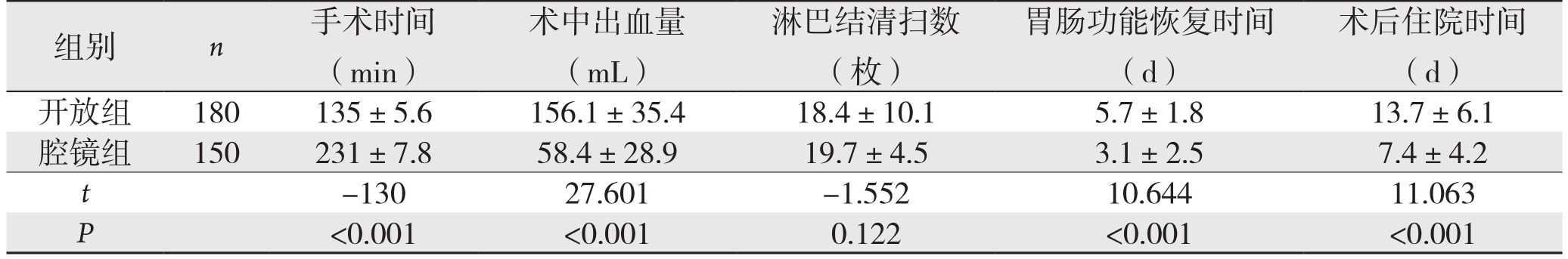
2.1 腔镜组与开放组患者的术中及术后各指标比较
腔镜组患者的手术时间明显长于开放组,术中出血量、术后肠道功能恢复时间及术后住院天数明显小于开放组,差异有统计学意义(均P<0.05);而两组的淋巴结清扫数目无统计学差异(P>0.05)(表2)。
表2 两组患者术中、术后指标比较( ±s)
±s)
Table 2 Comparison of the intra- and postoperative variable between the two groups of patients ( ±s)
±s)
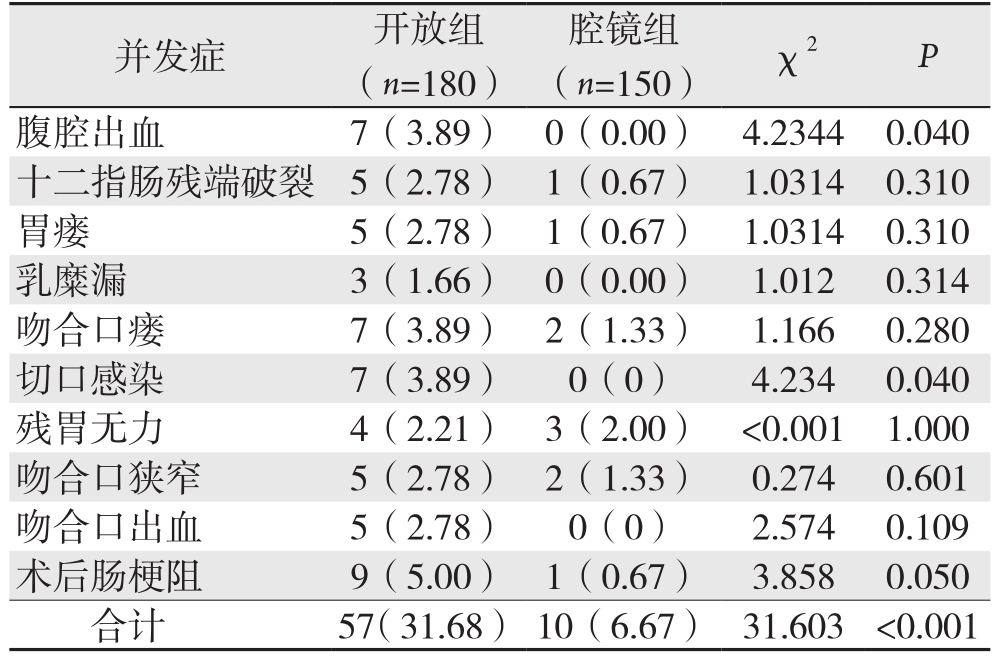
2.2 腔镜组与开放组患者的术后外科并发症比较
腔镜组的术后肠梗阻、腹腔出血、切口感染发生率以及外科并发症总发生率低于开放组,差异具有统计学意义(均P<0.05);而两组的十二指肠残端破裂、胃瘘、乳糜漏、吻合口瘘、残胃无力、吻合口狭窄、吻合口出血、发生率无统计学差异(均P>0.05)(表3)。
表3 两组患者术后外科并发症例次比较[n(%)]
Table 3 Comparison of the surgical complications between the two groups of patients [n (%)]
2.3 腔镜组和开放组患者的术后非外科并发症比较
开放组在皮下气肿及高碳酸血症优于腔镜组(均P<0.05),而两组的非外科并发症总发生率无统计学差异(P>0.05)(表4)。
2.4 腔镜组与开放组患者的总并发症发生率比较
腔镜组患者术后的总并发症发生率(8.67%)小于开放组(3 2.2 2%),差异有统计学意义(P<0.05)(表5)。
2.5 术后并发症影响因素的单变量分析
单变量分析显示,年龄、BMI、手术时间、术前患者血清蛋白及血红蛋白水平、肿瘤大小、淋巴结转移、术前合并症均与术后并发症的发生有关(均P<0.05);当患者年龄和体质量较大、手术时间长、术前营养状况差、肿瘤体积较大、术前存在合并症及出现淋巴结转移均会使手术的并发症增加(表6)。
表4 两组患者的术后非外科并发症例次比较[n(%)]
Table 4 Comparison of the non-surgical complications between the two groups of patients [n (%)]

表5 两组患者的总并发症发生率[n(%)]
Table 5 Comparison of overall complications between the two groups of patients [n (%)]

表6 术后并发症影响因素的单变量分析
Table 6 Univariate analysis of the influential factors for occurrence of complications

3 讨 论
随着科学技术的不断发展,内镜手术系统也随之应运而生。近些年各大医院的外科医生腹腔镜操作熟练度也在不断加强,腹腔镜手术广泛用于外科各个系统手术中[3-5]。例如腹腔镜下肾切除、肾部分切除、胆囊切除、阑尾切除及前列腺癌根治术等。然而由于胃部解剖的复杂性,使得该技术目前还未能在胃癌根治术中广泛开展利用,并且存在争议。首例早期胃癌实施腹腔镜胃癌根治术是由日本外科医生Kitano于1994年报道,后续并不断报道改术式情况[6-8],但由于胃癌在恶性肿瘤中病死率较高,患者及其家属在选择手术方式上较为慎重[9],而且胃部营养血管及侧支血管丰富、淋巴转移途径繁多等因素阻碍了腹腔镜胃癌手术的发展。因此,早期的胃癌根治性切除还是主张开放性手术,虽然该方法有显著的临床效果,基本能够达到手术无瘤原则,但对患者创伤大,术后恢复时间长,严重影响了该术式的进一步推广[10-13]。然而近年来,多篇报道[14-17]均提出了腹腔镜手术能够有效改善以上不足。近几年,腹腔镜胃癌根治技术的不断发展,该术式的适应证得以扩展,早期主要选择肿瘤分期早、瘤体小、手术简单的,现逐步扩展到进展期胃癌根治术,进而手术的难度也相应增加,随之带来的术后并发症也相应的增加。因此,分析常见并发症的影响因素是有效预防的关键。目前,关于胃癌根治术后的并发症主要包括:⑴ 外科并发症。胃瘘、残胃无力、十二指肠残端破裂、吻合口狭窄、腹腔出血、吻合口出血、乳糜漏、吻合口瘘、切口感染、术后肠梗阻等;⑵ 非外科并发症。皮下气肿、高碳酸血症、败血症、泌尿系感染、腹腔感染、肺部感染、深静脉栓塞等[18-21]。
本研究利用两组患者的临床资料进行了回顾性分析,比较两种术式的术中情况和术后并发症情况以及影响术后并发症的因素分析。结果显示,腔镜组的手术时间虽然显著长于开放组,但是腔镜组患者的术中出血量、胃肠功能恢复时间及术后住院天数均优于开放组;两组的淋巴结清扫数目方面差异无统计学意义,表明腔镜手术亦能够达到淋巴结清扫范围并能够保证手术切缘阴性,在保证临床治疗效果的同时能够减轻患者的创伤,加快患者术后康复。两种手术方式在分离解剖操作基本保持一致性,均是在指示下完成手术操作,进而均能相应降低术后并发症发生率[22-23]。韦斌等[24]研究报道证实,腹腔镜胃癌根治术治疗手术时间长于开腹胃癌根治术,但切口长度小于开腹胃癌根治术,且对应激反应影响小。徐丰等[25]研究报道证实,腹腔镜胃癌根治术治疗胃癌患者早期并发症发生率低,病死率低,具有较高的安全性。本研究中,通过对比两组的术后并发症发生率情况可知:腔镜组的并发症总发生率低于开放组(P<0.01),其中腔镜组在切口感染发生率、腹腔出血、术后肠梗阻上明显优于开放组,而开放组在皮下气肿及高碳酸血症上优于腔镜组;两组的十二指肠残端破裂、吻合口瘘、残胃无力、胃瘘、乳糜漏、吻合口狭窄、吻合口出血、肺部感染、泌尿系感染、腹腔感染、败血症、深静脉栓塞发生率均无统计学差异(P>0.05)。以上的研究结果可知,腹腔镜组手术患者手术切口较小减少了术后切口感染可能,术中视野清晰,解剖暴露真正实现骨骼化,使得出血量相应减少,术后胃肠功能恢复快,下床早,住院时间短。然而由于腔镜需要建立Trocar,通过腹腔二氧化碳的灌注保持视野的开放,进而导致了术后腔镜组的高碳酸血症及皮下气肿发生率高于开放组。再次总结两组的总并发症发生率的发生情况,可以发现腔镜组的术后并发症发生概率小于开放组,且差异具有统计学意义。总的来说,腹腔镜手术作为一种较新的术式,是一种安全有效的方法。除对比分析了两种手术方式的术中和术后并发症情况外,本研究对可能影响胃癌根治术后并发症发生率的其他危险因素做了单因素分析,结果提示手术时间、年龄、BMI、术前患者血清蛋白及血红蛋白水平、淋巴结转移情况、肿瘤大小、术前合并症均是影响因素。当患者年龄和体质量较大、手术时间长、术前营养状况差、肿瘤体积较大、术前存在合并症及出现淋巴结转移均会使手术的并发症增加。而有研究显示,手术的术后并发症能够显著影响患者围手术期恢复。
腹腔镜下胃癌根治术的创伤小,术后恢复快,总的并发症控制优于开放性手术,值得推广应用。腹腔镜胃癌根治术的日趋成熟,使得该术式的并发症逐步受到重视。想要更好的控制术后并发症,达到满意的临床效果,需要全面的了解腹腔镜胃癌根治术后各种并发症发生的原因,并熟知其影响因素,综合判断并掌握其防治措施,降低发生率。掌握以上,方能使腹腔镜胃癌根治术的手术效果及患者术后的恢复质量更好提升。
参考文献
[1]兰飞,谭晓俊.胃癌根治术后并发症的相关因素分析[J].中国现代医学杂志,2015,25(2):99–102.Lan F,Tan XJ.Related factors of complications of radicalsurgery for gastric cancer[J].China Journal of Modern Medicine,2015,25(2):99–102.
[2]World Health Organization (2014) GLOBOCAN2012:Estimated Cancer Incidence,Mortality and Prevalence Worldwide in 2012.http://globocan.iarc.fr/Default.aspx
[3]Kitano S,Iso Y,Moriyama M,et al.Laparoscopy-assisted Billroth I gastrectomy[J].Surg Laporosc Endosc,1994,4(2):146–148.
[4]Kim JW,Kim WS,Cheong JH,et al.Safety and efficacy of fasttrack surgery in laparoscopic distal gastrectomy for gastric cancer:a randomized clinical trial[J].World J Surg,2012,36(12):2879–2887.doi:10.1007/s00268–012–1741–7.
[5]Yoshikawa T,Fukunaga T,Taguri M,et al.Laparoscopic or open distal gastrectomy after neoadjuvant chemotherapy for operable gastric cancer,a randomized Phase II trial (LANDSCOPE trial) [J].Jpn J Clin Oncol,2012,42(7):654–657.
[6]陈哲,任双义.腹腔镜辅助下胃癌根治术疗效分析[J].中华腔镜外科杂志:电子版,2014,7(6):10–13.doi:10.3877/cma.j.issn.1674–6899.2014.06.004.Chen Z,Ren SY.Comparison of the clinical outcomes between laparoscopic gastrectomy and open gastrectomy for advanced gastric cancer[J].Chinese Journal of Laparoscopic Surgery:Electronic Edition,2014,7(6):10–13.doi:10.3877/cma.j.issn.1674–6899.2014.06.004.
[7]李东虎.腹腔镜辅助胃癌根治术50例临床疗效分析[J].中国实用医药,2015,10(7):95–96.doi:10.14163/j.cnki.11–5547/r.2015.07.064.Li DH.Clinical efficacy of laparoscopic-assisted radical gastrectomy:an analysis in 50 cases[J].China Practical Medical,2015,10(7):95–96.doi:10.14163/j.cnki.11–5547/r.2015.07.064.
[8]Okabe H,Tsunoda S,Obama K,et al.Feasibility of Laparoscopic Radical Gastrectomy for Gastric Cancer of Clinical Stage II or Higher:Early Outcomes in a Phase II Study (KUGC04)[J].Ann Surg Oncol,2016,23(Suppl 4):516–523.
[9]梁阔,刘东斌,刘家峰,等.腹腔镜胆总管探查一期缝合治疗老年胆总管结石的临床疗效分析[J].中国普通外科杂志,2017,26(8):1030–1035.doi:10.3978/j.issn.1005–6947.2017.08.011.Liang K,Liu DB,Liu JF,et al.Clinical efficacy of laparoscopic common bile duct exploration with primary closure for choledocholithiasis in elderly patients[J].Chinese Journal of General Surgery,2017,26(8):1030–1035.doi:10.3978/j.issn.1005–6947.2017.08.011.
[10]刘斌.胃癌根治术前行动脉介入化疗与单纯胃癌根治术治疗进展期胃癌的对照研究[J].海南医学院学报,2016,22(2):182–185.doi:10.13210/j.cnki.jhmu.20151021.011.Liu B.Control study of arterial interventional chemotherapy before radical gastrectomy for gastric cancer and simple radical gastrectomy for gastric cancer in treatment of advanced gastric cancer[J].Journal of Hainan Medical University,2016,22(2):182–185.doi:10.13210/j.cnki.jhmu.20151021.011.
[11]黄晓明,陈培浩.腹腔镜下胃癌根治术与开放性胃癌根治术的差异分析[J].临床医学工程,2016,23(4):417–418.doi:10.3969/j.issn.1674–4659.2016.04.0417.Huang XM,Chen PH.Analysis on the difference of laparoscopic radical gastrectomy and open radical gastrectomy[J].Clinical Medical &Engineering,2016,23(4):417–418.doi:10.3969/j.issn.1674–4659.2016.04.0417.
[12]任俭,崔建民,金晓军.腹腔镜和开放胃癌根治术的疗效比较[J].齐齐哈尔医学院学报,2015,36(32):4847–4849.Ren J,Cui JM,Jin XJ.Comparison of effect of laparoscopic with open radical gastrectomy for gastric cancer[J].Journal of Qiqihar University of Medicine,2015,36(32):4847–4849.
[13]赵庆洪,鲁明,张弛,等.腹腔镜胃癌根治术与开放性胃癌根治术的对比研究[J].临床肿瘤学杂志,2010,15(5):438–440.doi:10.3969/j.issn.1009–0460.2010.05.014.Zhao QH,Lu M,Zhang C,et al.Comparative study of laparoscopic gastrectomy and open gastrectomy for gastric cancer[J].Chinese Clinical Oncology,2010,15(5):438–440.doi:10.3969/j.issn.1009–0460.2010.05.014.
[14]邱俊然,李英儒.腹腔镜下胃癌根治术与开放性胃癌根治术的对比分析[J].实用中西医结合临床,2015,15(9):29–30.doi:10.13638/j.issn.1671–4040.2015.09.016.Qiu JR,Li YR.Comparison of laparoscopic and open radical gastrectomy[J].Practical Clinical Journal of Integrated Traditional Chinese and Western Medicine,2015,15(9):29–30.doi:10.13638/j.issn.1671–4040.2015.09.016.
[15]郑朝辉,陆俊,黄昌明,等.胃癌根治术后并发症及其相关因素分析[J].中国实用外科杂志,2013,33(4):317–320.Zheng CH,Lu J,Huang CM,et al.Postoperative complications and the risk factors of radical gastrectomy for gastric cancer[J].Chinese Journal of Practical Surgery,2013,33(4):317–320.
[16]冯之良.腹腔镜下胃癌根治术的手术配合及效果分析[J].深圳中西医结合杂志,2014,24(8):141–142.Feng ZL.Operative cooperation and its efficacy in laparoscopic radical gastrectomy[J].Shenzhen Journal of Integrated Traditional Chinese and Western Medicine,2014,24(8):141–142.
[17]Bencivenga M,Verlato G,Han DS,et al.Validation of two prognostic models for recurrence and survival after radical gastrectomy for gastric cancer[J].Br J Surg,2017,104(9):1235–1243.doi:10.1002/bjs.10551.
[18]Inaoka K,Kanda M,Uda H,et al Clinical utility of the plateletlymphocyte ratio as a predictor of postoperative complications after radical gastrectomy for clinical T2–4 gastric cancer[J].World J Gastroenterol,2017,23(14):2519–2526.doi:10.3748/wjg.v23.i14.2519.
[19]Huang DD,Zhou CJ,Wang SL,et al.Impact of different sarcopenia stages on the postoperative outcomes after radical gastrectomy for gastric cancer[J].Surgery,2017,161(3):680–693.doi:10.1016/j.surg.2016.08.030.
[20]陈雷,王志刚,雷泽华,等.全腔镜与开腹远端胃癌D2根治术的疗效及对免疫功能影响的比较研究[J].中国普通外科杂志,2016,25(4):558–564.doi:10.3978/j.issn.1005–6947.2016.04.016.Chen L,Wang ZG,Lei ZH,et al.Totally laparoscopic versus open distal radical gastrectomy with D2 dissection:the efficacy and im pact on immune function[J].Chinese Journal of General Surgery,2016,25(4):558–564.doi:10.3978/j.issn.1005–6947.2016.04.016.
[21]Li HZ,Chen JX,Zheng Y,et al.Laparoscopic-assisted versus open radical gastrectomy for resectable gastric cancer:Systematic review,meta-analysis,and trial sequential analysis of randomized controlled trials[J].J Surg Oncol,2016,113(7):756–767.doi:10.1002/jso.24243.
[22]Shi RL,Chen Q,Ding J B,et al.Increased number of negative lymph nodes is associated with improved survival outcome in node positive gastric cancer following radical gastrectomy[J].Oncotarget,2016,7(23):35084–35091.doi:10.18632/oncotarget.9041.
[23]Kanaji S,Suzuki S,Yamamoto M,et al.Radical Lymph Node Dissection Along the Proximal Splenic Artery During Laparoscopic Gastrectomy for Gastric Cancer Using the Left Lateral Approach[J].Ann Surg Oncol,2017,24(9):2727.doi:10.1245/s10434–017–5877–4.
[24]韦斌,黄顺荣,钟晓刚,等.腹腔镜胃癌根治术与开腹胃癌根治术对患者应激炎性因子影响的对比分析[J].中国临床医生,2014,42(10):25–27.doi:10.3969/j.issn.1008–1089.2014.10.08.Wei B,Huang SR,Zhong XG,et al.Comparison and analysis of laparoscopic and open radical gastrectomy for gastric cancer surgery in patients with stress-inflammatory factor[J].Chinese Journal for Clinicians,2014,42(10):25–27.doi:10.3969/j.issn.1008–1089.2014.10.08.
[25]徐丰,吴剑宏,冯永东等.腹腔镜胃癌根治术819例术后早期并发症的分析及防治[J].中华临床医师杂志:电子版,2014,8(24):4336–4340.doi:10.3877/cma.j.issn.1674–0785.2014.24.005.Xu F,Wu JH,Feng YD,et al.Analysis and prevention of early postoperative complications of 819 cases of laparoscopic radical gastrectomy[J].Chinese Journal of Clinicians:Electronic Edition,2014,8(24):4336–4340.doi:10.3877/cma.j.issn.1674–0785.2014.24.005.
