甲状腺乳头状癌是头颈部外科最常见的恶性肿瘤之一,近年来发病率呈逐年上升的趋势,现约占甲状腺癌的85%左右[1]。甲状腺微小乳头状癌(papillary thyroid microcarcinoma,PTMC)是指最大直径≤1 cm的肿瘤,一般认为具有较低侵袭性和淋巴结转移率,其术后生存率亦较非PTMC更好[2]。多灶性甲状腺乳头状癌(multifocal papillary thyroid carcinoma,MPTC)是指病灶数目≥ 2个的甲状腺乳头状癌,是甲状腺癌的重要临床特点之一[3]。目前多灶性PTMC是甲状腺外科医生需要面对的重要课题之一,其临床病理特征、治疗和预后尚缺乏深入的研究。中南大学湘雅医院2013年7月—2016年12月共收治270例PTMC,其中120例为多灶性PTMC。本文回顾性分析120例多灶性PTMC的临床资料,探讨多灶PTMC的临床特点和预防性中央区淋巴结清扫的意义。
1 资料与方法
1.1 一般资料
将2013年7月—2016年12月收治的270例PTMC患者中120例多灶PTMC的临床资料和手术结果分析研究。纳入研究的患者均为初次发病者,患者既往无颈部手术、甲状腺消融及外伤史。所有患者术前均行彩色超声评估甲状腺结节,基于患者意愿和临床因素,术前对影像学怀疑恶性,肿瘤直径≥5 mm的病灶行细针穿刺活检(fine needle aspiration biopsy,FNAB)结果显示为可疑恶性或恶性。触诊和彩超评估颈部淋巴结无术前转移淋巴结征象。所有患者经术后石蜡切片证实甲状腺内有2个或2个以上的病灶,其中病灶最大直径<1 cm。14例患者术前各项评估考虑为单发病灶,但经术中冷冻切片和术后石蜡切片确诊为多灶PTMC。
所有患者均行全/近全甲状腺切除,术中冷冻切片证实为多灶性甲状腺微小乳头状癌。全部病灶位于一侧甲状腺腺叶者行患侧中央区淋巴结清扫,病灶分布于双侧腺叶者则行双侧中央区淋巴结清扫术。术中全程暴露喉返神经并加以保护;原位保留甲状旁腺,必要时行甲状旁腺自体移植。中央区淋巴结清扫包括喉前、气管前、气管旁和气管食管沟的淋巴脂肪,右侧中央区注意清扫喉返神经后方淋巴脂肪组织。
1.2 观察指标
统计和比较全部纳入研究的患者年龄,性别,原发肿瘤直径、数目,是否分布于双侧,是否侵犯包膜,有无中央区淋巴结转移和转移情况等临床病理特征。比较分析多灶性PTMC和单灶性PTMC的临床病理特征,研究影响中央区淋巴结转移的因素。
1.3 统计学处理
采用SPSS 16.5软件对两组所得的数据进行统计分析,一般资料用均数±标准差( ±s)的形式表示。计量资料采用t检验,计数资料比较采用χ2检验,P<0.05 为差异有统计学意义。
±s)的形式表示。计量资料采用t检验,计数资料比较采用χ2检验,P<0.05 为差异有统计学意义。
2 结 果
2.1 多灶性PTMC临床病理特征
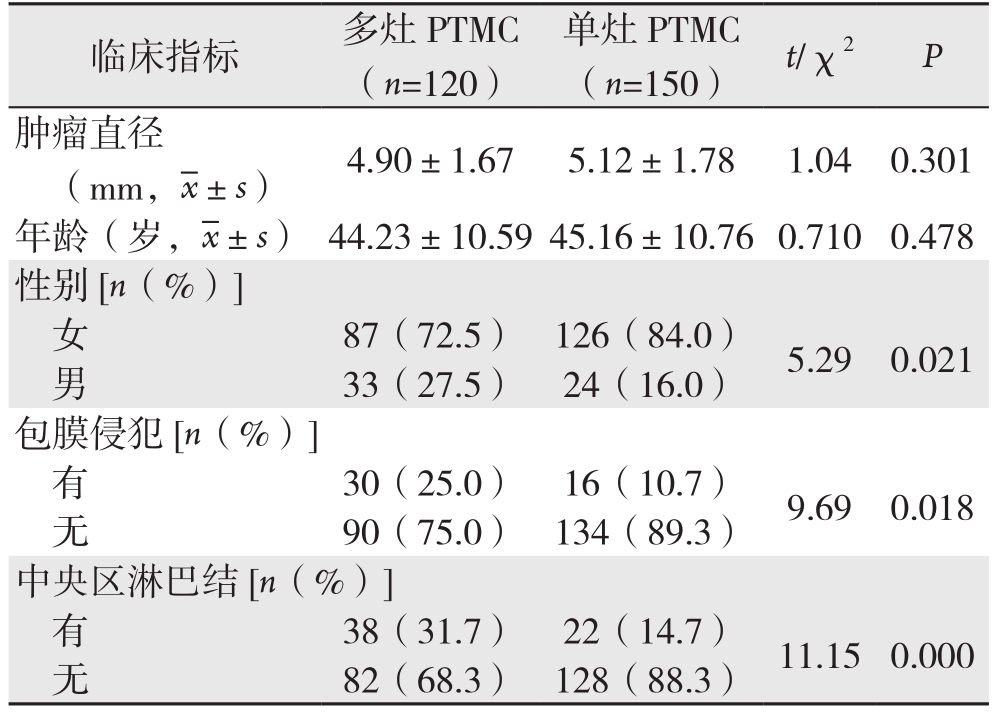
本组120例患者中男33例,女87例;年龄23~68岁,平均年龄(44.23±10.59)岁;肿瘤直径1~10 mm,平均直径(4.90±1.67)mm;病灶位于甲状腺单侧腺叶者38例(31.67%),位于双侧腺叶者82例(68.33%);30例(25.0%)经术后病理证实肿瘤侵犯甲状腺包膜。术前临床考虑为单灶,术中、术后病理证实为多灶的14例(11.67%)。38例(31.67%)患者存在中央区淋巴结转移,其中双侧转移24例(20.0%),单侧转移14例(11.67%)。多灶性与单灶性PTMC在发病年龄、单个肿瘤直径上无统计学差异(P>0.05);与单灶性PTMC相比,多灶性PTMC在男性患者中比例较高、更容易出现包膜侵犯(均P<0.05),且更容易发生中央区淋巴结的转移(P<0.01)(表1)。
表1 多灶PTMC与单灶PTMC患者临床资料比较
Table 1 Comparison of the clinical data between multifocal and unifocal PTMC patients
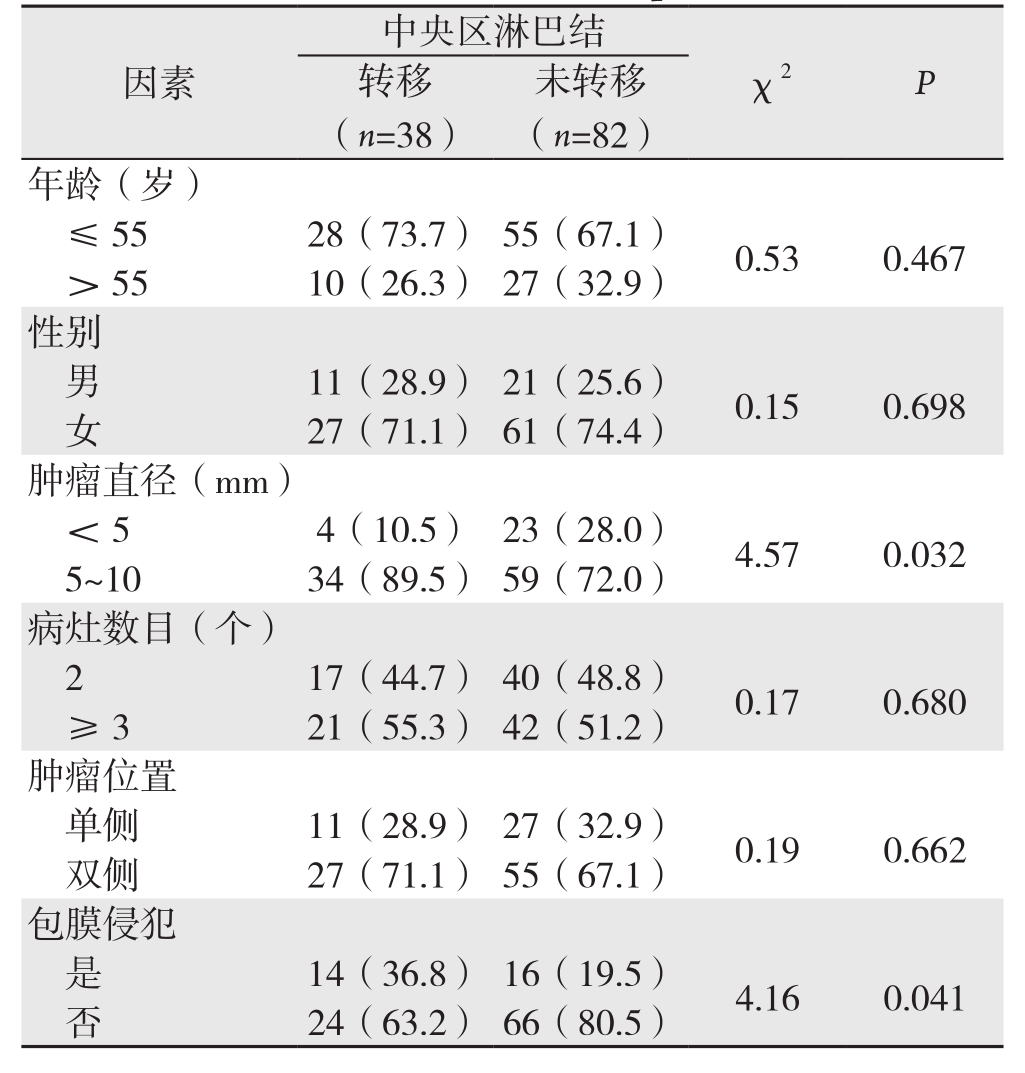
2.2 多灶性PTMC中央区淋巴结转移的相关因素分析
分析临床病理因素包括年龄、性别、肿瘤最大直径、病灶数目、病灶分布和是否侵犯甲状腺包膜与中央区淋巴结转移的关系。结果显示:中央区淋巴结转移的发生与患者年龄和性别无关(均P>0.05);肿瘤最大直径5~10 mm者较<5 mm者中央区淋巴结转移发生率明显升高(P<0.05);肿瘤侵犯包膜者更容易出现中央区淋巴结转移(P<0.05);多灶PTMC肿瘤数目(2 vs. ≥3)和分布(单侧 vs. 双侧)与中央区淋巴结转移发生率无关(均P>0.05)(表2)。
表2 多灶PTMC患者临床因素与中央区淋巴结转移关系[n(%)]
Table 2 Relations of clinical factors with central lymph node metastasis in multifocal PTMC patients [n (%)]
中央区淋巴结未转移(n=82)年龄(岁)≤55 28(73.7) 55(67.1) 0.53 0.467> 55 10(26.3) 27(32.9)性别男11(28.9) 21(25.6) 0.15 0.698女27(71.1) 61(74.4)肿瘤直径(mm)<5 4(10.5) 23(28.0) 4.57 0.032 5~10 34(89.5) 59(72.0)病灶数目(个)2 17(44.7) 40(48.8) 0.17 0.680≥ 3 21(55.3) 42(51.2)肿瘤位置单侧 11(28.9) 27(32.9) 0.19 0.662双侧 27(71.1) 55(67.1)包膜侵犯是14(36.8) 16(19.5) 4.16 0.041否24(63.2) 66(80.5)因素 χ2 P转移(n=38)
2.3 术后并发症发生情况
120例患者术后并发症发生6例。术后暂时性低钙血症3例(2.5%),1个月后复查血钙和PTH均恢复正常。暂时性声带麻痹2例(1.67%),3个月后复查声带活动和发音均恢复正常。术后皮下出血1例(0.83%),经局部压迫及切口处引流后好转。无永久性喉返神经麻痹和永久性甲状旁腺功能低下,无死亡病例。
3 讨 论
近年来甲状腺乳头状癌发病率的迅速上升,其中有约50%以上归因于甲状腺微小乳头状癌(PTMC)的增长[4-5]。临床上PTMC具有较低的术后复发率约1%~5%,如果仅统计CN0期患者则其复发率低至1%以下[6-7]。基于PTMC惰性的生物学行为和良好的预后,甚至有研究[8-10]提出对低危PTMC患者可以进行严密的动态监测。多灶性作为甲状腺乳头状癌的重要临床特征,根据不同的报道其发病率约为18%~87%[11]。研究[12]表明多发病灶具有较高的包膜侵犯率和淋巴转移发生率,其是甲状腺乳头状癌残存和复发的独立高风险因素。因此,多灶PTMC临床病理的特点和对其手术方式的选择逐渐成为研究的热点之一。
多灶性PTMC兼具甲状腺乳头状微小癌和多灶性的临床特性,越来越多地引起外科医生的关注。So等[13]报道多灶性甲状腺微小乳头状癌的发生率为36.1%。本组患者中多灶性PTMC 44.4%(120/270),略高于文献报道。多数研究[11,14]显示多灶与单灶甲状腺乳头状癌中性别比例和年龄比较没有差异。本组结果显示多灶组PTMC中男性的发病率要高于单灶组PTMC(27.5% vs. 16.0%,P=0.021);而两者在年龄上则无统计学差异,这与单志东等[15]研究结果一致。研究[16]显示多灶PTMC的肿瘤平均直径明显小于单灶PTMC的肿瘤直径,而将多灶PTMC分成2个和≥3个病灶组是则无显著差异。本组结果显示多灶组的肿瘤平均直径小于单灶组,但两者无统计学差异(P=0.301)。多灶PTMC位于双侧腺叶的比率为69.6%,而且单侧多发PTMC比单侧单发PTMC对侧微小癌的发生率会成倍增加(69.1% vs. 29.6%)[17-19]。本组多灶性PTMC位于双侧者占68.3%,与上述研究结果一致。有报道[20]称5.5%~21.3%的多灶PTMC患者存在常规术前B超检查和穿刺细胞学活检未能发现的隐匿病灶,这是造成术后的漏诊和复发的主要因素。本组亦有14例术前临床考虑为单灶,术后病理确诊为多灶。说明多灶PTMC中常合并存在一些极其微小不易被发现的潜在病灶,可以局限一侧腺叶,也可以位于两侧。包膜侵犯是甲状腺乳头状癌淋巴结转移和预后风险因素之一,在多灶性PTMC的发生率显著高于单灶性PTMC[9,11,19]。Kim等[12]研究多灶性PTMC的中央区淋巴结转移发生率为42.1%,明显高于单灶性(28.1%)。本组资料显示多灶性PTMC的包膜侵犯和中央区淋巴结转移发生率均显著高于单灶组PTMC,与前述研究结果一致。
中央区淋巴结转移是甲状腺癌的主要转移途径之一,同时也是复发和远处转移的危险因素之一[21-22]。C N0期P T M C中央区淋巴结转移发生率约3 3%左右,而多灶P T M C颈淋巴结转移率则可高达5 5.6%[23-24]。本组数据显示对于C N0的患者进行预防性中央区淋巴结清扫,淋巴结转移发生率(3 8/1 2 0,3 1.7%)。Z h a n g等[25]研究显示P T M C的中央区淋巴结转移与男性、年龄(≤4 5岁)、多灶性、腺外侵犯和大小(>6 m m)密切相关。而目前多项研究建议将分期中的年龄切点值由45岁增至55岁[26-27],美国癌症联合委员会(American Joint Committee on Cancer AJCC)最新甲状腺癌分期也已将年龄界限更改为55岁,因此我们分析性别及年龄(55岁为界限)对中央区淋巴结转移的影响,未见明显差异(P>0.05)。通常认为直径越大的肿瘤发生淋巴结转移的风险越大,本研究在对5~10 mm与<5 mm的病灶对比中发现,5~10 mm的病灶发生中央区淋巴结转移风险更高(P=0.032)。也有部分学者[28]把这个临界值定在7mm,认为<5 mm与5~7 mm之间病灶比较中央区淋巴结转移无明显差异。Tam等[14]研究显示随病灶数目的增加淋巴结转移发生率亦逐渐升高,病灶数为1、2、3和4个的淋巴结转移发生率分别为6.5%、10.5%、13.6%和19.2%。本组比较病灶的数目(2 vs. ≥3)和分布(单侧vs. 双侧)与中央区淋巴结转移发生率的关系,结果显示没有差异,这可能与病例分组和例数有关。本组结果显示包膜侵犯明显增加中央区淋巴结转移发生率(P<0.05),这与大多数研究[11,13-14,25]结果一致。多数研究[29-30]证实中央区淋巴结清扫并不增加永久性甲状旁腺功能低下和永久性声带麻痹。本组术后并发症例数6例(5%)包括3例术后暂时性低钙血症(2.5%)和2例暂时性声带麻痹(1.67%),无永久性喉返神经麻痹和永久性甲状旁腺功能低下。
综上所述,多灶性PTMC与单灶性PTMC相比包膜侵犯和中央区淋巴结转移的发生率更高。多灶PTMC行预防性中央区淋巴结清扫术是很有必要的,尤其是最大肿瘤直径>5mm和出现包膜侵犯者。
参考文献
[1]Yin DT, Xu J, Lei M, et al. Characterization of the novel tumorsuppressor gene CCDC67 in papillary thyroid carcinoma [J].Oncotarget, 2016, 7(5):5830–5841. doi: 10.18632/oncotarget.6709.
[2]Lo CY,Chan WF, Lang BH, et al. Papillary microcarcinoma: is there any difference between clinically overt and occult tumors?[J].World J Surg, 2006, 30(5):759–766.
[3]Wang W, Su X, He K, et al. Comparison of the clinicopathologic features and prognosis of bilateral versus unilateral multifocal papillary thyroid cancer: An updated study with more than 2000 consecutive patients[J]. Cancer, 2016, 122(2):198–206. doi:10.1002/cncr.29689.
[4]Enewold LR, Zhou J, Devesa SS, et al. Thyroid cancer incidence among active duty U.S. military personnel, 1990–2004[J]. Cancer Epidemiol Biomarkers Prev, 2011, 20(11):2369–2376. doi:10.1158/1055–9965.EPI-11–0596.
[5]Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002[J]. JAMA, 2006, 295(18):2164–2167.
[6]Leboulleux S, Tuttle RM, Pacini F, et al. Papillary thyroid microcarcinoma: time to shift from surgery to active surveillance?[J]. Lancet Diabetes Endocrinol, 2016, 4(11):933–942.doi: 10.1016/S2213–8587(16)30180–2.
[7]Wada N, Duh QY, Sugino K,et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection[J]. Ann Surg, 2003, 237(3):399–407. Epub 2003/03/05.
[8]Haser GC, Tuttle RM, Su HK, et al. Active Surveillance for Papillary Thyroid Microcarcinoma: New Challenges and Opportunities for the Health Care System[J]. Endocr Pract, 2016,22(5):602–611. doi: 10.4158/EP151065.RA.
[9]Ito Y, Miyauchi A, Oda H. Low-risk papillary microcarcinoma of the thyroid: A review of active surveillance trials[J]. Eur J Surg Oncol, 2017, pii: S0748–7983(17)30370–0. doi: 10.1016/j.ejso.2017.03.004. [Epub ahead of print]
[10]中国抗癌协会甲状腺癌专业委员会(CATO). 甲状腺微小乳头状癌诊断与治疗中国专家共识 (2016版)[J]. 中国肿瘤临床, 2016,43(10):405–411. doi:10.3969/j.issn.1000–8179.2016.10.001.Chinese Association of Thyroid Oncology (CATO). Chinese experts consensus on diagnosis and treatment of papillary thyroid microcarcinoma (2016 edition)[J]. Chinese Journal of Clinical Oncology, 2016, 43(10):405–411. doi:10.3969/j.issn.1000–8179.2016.10.001.
[11]Iacobone M, Jansson S, Barczyński M, et al. Multifocal papillary thyroid carcinoma--a consensus report of the European Society of Endocrine Surgeons (ESES)[J]. Langenbecks Arch Surg, 2014,399(2):141–154. doi: 10.1007/s00423–013–1145–7.
[12]Kim HJ, Sohn SY, Jang HW, et al. Multifocality, but not bilaterality,is a predictor of disease recurrence/persistence of papillary thyroid carcinoma[J]. World J Surg, 2013, 37(2):376–384. doi: 10.1007/s00268–012–1835–2.
[13]So YK, Kim MW, Son YI. Multifocality and bilaterality of papillary thyroid microcarcinoma[J]. Clin Exp Otorhinolaryngol, 2015,8(2):174–178. doi: 10.3342/ceo.2015.8.2.174.
[14]Tam AA, Özdemir D, Çuhacı N, et al. Association of multifocality,tumor number, and total tumor diameter with clinicopathological features in papillary thyroid cancer[J]. Endocrine, 2016, 53(3):774–783. doi: 10.1007/s12020–016–0955–0.
[15]单志东, 巩鹏, 王忠裕. 多灶性甲状腺乳头状癌的构成比变化及临床分析[J]. 国际外科学杂志, 2013, 40(5):306–310. doi:10.3760/cma.j.issn.1673–4203.2013.05.007.Shan ZD, Gong P, Wang ZY. Change of constituent ratio and clinical analysis of multifocal papillary thyroid carcinoma[J].International Journal of Surgery, 2013, 40(5):306–310. doi:10.3760/cma.j.issn.1673–4203.2013.05.007.
[16]严丽, 李情怀, 王树峰, 等. 术前TSH水平与甲状腺结节良恶性关系[J]. 中国普通外科杂志, 2012, 21(11):1373–1376.Yan L, Li QH, Wang SF, et al. Relationship between preoperative serum thyrotropin (TSH) level and the nature of thyroid nodule[J].Chinese Journal of General Surgery, 2012, 21(11):1373–1376.
[17]林琳, 郑向前, 刘磊, 等. 多灶性甲状腺乳头状癌的生物学特性及治疗分析[J]. 中华普通外科杂志, 2010, 25(8):621–623. doi:10.3760/cma.j.issn.1007–631X.2010.08.006.Lin L, Zheng XQ, Liu L, et al. Multifocal papillary thyroid carcinoma[J]. Zhong Hua Pu Tong Wai Ke Za Zhi, 2010, 25(8):621–623. doi:10.3760/cma.j.issn.1007–631X.2010.08.006.
[18]Kim ES, Kim TY, Koh JM,et al. Completion thyroidectomy in patients with thyroid cancer who initially underwent unilateral operation[J]. Clin Endocrinol (Oxf), 2004, 61(1):145–148.
[19]殷德涛, 韩飏, 张亚原, 等. 多灶性甲状腺乳头状癌的临床病理及颈淋巴结转移特征[J]. 中国普通外科杂志, 2017, 26(5):556–560.doi:10.3978/j.issn.1005–6947.2017.05.004.Yin DT, Han Y, Zhang YY, et al. Clinicopathologic and neck metastasis features of multifocal papillary thyroid cancer[J].Chinese Journal of General Surgery, 2017, 26(5):556–560.doi:10.3978/j.issn.1005–6947.2017.05.004.
[20]Koo BS, Lim HS, Lim YC, et al. Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma[J]. Ann Surg Oncol, 2010, 17(4):1101–1105. doi: 10.1245/s10434–009–0906–6.
[21]Mercante G, Frasoldati A, Pedroni C, et al. Prognostic factors affecting neck lymph node recurrence and distant metastasis in papillary microcarcinoma of the thyroid: results of a study in 445 patients[J]. Thyroid, 2009, 19(7):707–716. doi: 10.1089/thy.2008.0270.
[22]孟庆东, 边学海, 孙辉. 多灶性甲状腺乳头状癌的诊疗进展[J].中国普通外科杂志, 2016, 25(11):1640–1645. doi:10.3978/j.issn.1005–6947.2016.11.020.Meng QD, Bian XH, Sun H. Diagnosis and treatment of multifocal papillary thyroid carcinoma: recent progress[J]. Chinese Journal of General Surgery, 2016, 25(11):1640–1645. doi:10.3978/j.issn.1005–6947.2016.11.020.
[23]Liu LS, Liang J, Li JH, et al. The incidence and risk factors for central lymph node metastasis in cN0 papillary thyroid microcarcinoma: a meta-analysis[J]. Eur Arch Otorhinolaryngol,2017, 274(3):1327–1338. doi: 10.1007/s00405–016–4302–0.
[24]Zhao Q, Ming J, Liu C, et al. Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma[J]. Ann Surg Oncol, 2013, 20(3):746–752. doi:10.1245/s10434–012–2654–2.
[25]Zhang L, Wei WJ, Ji QH, et al. Risk factors for neck nodal metastasis in papillary thyroid microcarcinoma: a study of 1066 patients[J]. J Clin Endocrinol Metab, 2012, 97(4):1250–1257. doi:10.1210/jc.2011–1546.
[26]Ganly I, Nixon IJ, Wang LY, et al. Survival from differentiated thyroid cancer: What has age got to do with it ?[J]. Thyroid, 2015,25(10):1106–1114. doi: 10.1089/thy.2015.0104.
[27]Nixon IJ, Kuk D, Wreesmann V, et al. De fi ning a valid age cutoffin staging of well-differentiated thyroid cancer[J]. Ann Surg Oncol,2016, 23(2):410–415. doi: 10.1245/s10434–015–4762–2.
[28]Lee KJ, Cho YJ, Kim SJ, et al. Analysis of the clinicopathologic features of papillary thyroid microcarcinoma based on 7-mm tumor size[J]. World J Surg, 2011, 35(2):318–323. doi: 10.1007/s00268–010–0886–5.
[29]Yoo HS, Shin MC, Ji YB, et al. Optimal extent of prophylactic central neck dissection for papillary thyroid carcinoma: Comparison of unilateral versus bilateral central neck dissection[J]. Asian J Surg, 2017, pii: S1015–9584(17)30011–8. doi: 10.1016/j.asjsur.2017.03.002. [Epub ahead of print]
[30]Seo GH, Chai YJ, Choi HJ, et al. Incidence of permanent hypocalcaemia after total thyroidectomy with or without central neck dissection for thyroid carcinoma: a nationwide claim study[J].Clin Endocrinol (Oxf), 2016, 85(3):483–487. doi: 10.1111/cen.13082.