随着介入技术发展,胸主动脉覆膜支架腔内修复术(thoracic endovascular aortic repair,TEVAR)逐渐成为了主动脉弓降部疾病的首选治疗方式[1-2]。当近端锚定区不足,即病变距离左侧锁骨下动脉开口较近时,为获得足够的近端锚定区,确保主动脉弓降部病变被完整覆盖,将左侧锁骨下动脉开口直接封堵是业界学者经常采用的处理方式,尤其是对于非左椎动脉优势的患者而言。尽管临床经验显示,部分患者术后会产生一定后遗症,如左上肢缺血症状,但也有研究[3]显示左侧锁骨下动脉开口被覆盖并不会明显增加手术风险,更加使得这一简便快捷的手段得以广泛应用。
对于需行冠状动脉旁路移植手术的患者而言,目前最常用的心肌再血管化手术方式是采用左锁骨下动脉的分支——左乳内动脉作为血管移植物,行冠脉左前降支的旁路移植手术,其余靶血管则选用1支或多支大隐静脉以“升主动脉-大隐静脉-冠脉靶血管”的方式搭桥。由于动脉桥的长期通畅率远高于大隐静脉,左乳内动脉桥成为了最为重要的冠状动脉前降支桥血管的第一选择和最佳选择,对患者长期生存的影响意义重大[4]。
因此,对于合并严重冠心病,已经接受左乳内动脉-冠脉前降支搭桥或即将接受冠状动脉旁路移植手术的主动脉弓降部疾病患者而言,在实施TEAVR手术过程中,保留左锁骨下动脉进而保证左乳内动脉血供具有重要意义。笔者回顾性分析9例合并严重冠心病并且近端锚定区≤1 cm 的主动脉弓降部疾病患者资料,针对锚定区不足的特殊患者,如何采取措施保证左锁骨下动脉血供进行探讨。
1 资料与方法
1.1 一般资料
回顾性分析2016年4月—2016年7月期间,阜外医院血管外科收治的9例合并严重冠心病并且近端锚定区≤1 cm的主动脉弓降部疾病患者资料。9例患者,男7例,女2例;平均年龄60(37~76)岁,全部接受胸主动脉腔内修复术治疗。由于本组患者合并严重冠心病,已经接受或未来短期内可能接受左乳内动脉-冠状动脉前降支旁路移植手术治疗,因此均需保留左锁骨下动脉,从而保留作为冠脉前降支桥血管最佳来源的左乳内动脉。本组患者术前患有高血压病史7例,高血脂病史6例,糖尿病史1例,既往经皮冠状动脉支架植入(PCI)手术史5例,既往冠状动脉旁路移植手术史4例。
1.2 治疗方法
所有患者均在全麻下行TEVAR手术。常规行腹股沟上方斜切口游离暴露右侧股动脉,穿刺并逆行置入导丝导管至升主动脉,造影确认主动脉弓降部病变性质及其大小、位置、形态,测量主动脉锚定区口径、病变与左锁骨下动脉距离等,根据测量结果选取合适口径的主动脉覆膜支架。再经股动脉导人覆膜支架输送器,到达理想位置后释放主动脉覆膜支架。
对于近端锚定区不足、必须覆盖左侧锁骨下动脉的患者,行左锁骨下动脉“烟囱”支架植入术。即在TEVAR术中使用Fluency覆膜支架(巴德,美国)作为“烟囱”支架,保留左侧锁骨下动脉血供并增加主动脉覆膜支架近端锚定区。“烟囱”支架的型号选择及释放位置以其近端超过主动脉覆膜支架覆膜部分前缘1~2 cm,远端避免覆盖左侧椎动脉和左乳内动脉为准。两枚支架的释放顺序为:先经肱动脉预置“烟囱”支架至上述理想位置不释放,待主动脉覆膜支架释放完毕后,再释放“烟囱”支架并辅以球囊扩张以确保其通畅性。再次造影判断病变是否被完全隔绝,左锁骨下动脉是否得以保留。
1.3 疗效评价
从乳内动脉保留成功率、生存率、并发症发生率等来评价腔内治疗的预后。
2 结 果
2.1 患者手术情况
9例合并严重冠心病并且近端锚定区不足的患者接受TEVAR治疗,采用的主动脉移植物包括Aukura覆膜支架(先健,中国)3例和Valiant覆膜支架(美敦力,美国)6例。其中4例有冠状动脉旁路移植手术史的患者,均接受过左乳内动脉-前降支旁路移植,主动脉弓降部病变位置距离左锁骨下动脉仅为5~10 mm,主动脉覆膜支架均直接锚定于左锁骨下动脉开口以远并紧邻左锁骨下动脉释放,将弓降部病变完整覆盖,同时保留左锁骨下动脉;5例暂未行冠状动脉旁路移植手术的患者,2例也按照上述方式直接实施TEVAR手术,成功将主动脉覆膜支架精准锚定于左锁骨下动脉以远,3例锚定区为0~8 mm,术中严密评估后认为无法保证在实施TEVAR手术时左锁骨下动脉开口不被覆盖,其中2例同期加行左锁骨下动脉“烟囱”支架植入术(图1),另1例行TEVAR手术、左锁骨下动脉“烟囱”支架植入术的同时,由于髂动脉病变严重,还实施了髂动脉人工血管置换术。
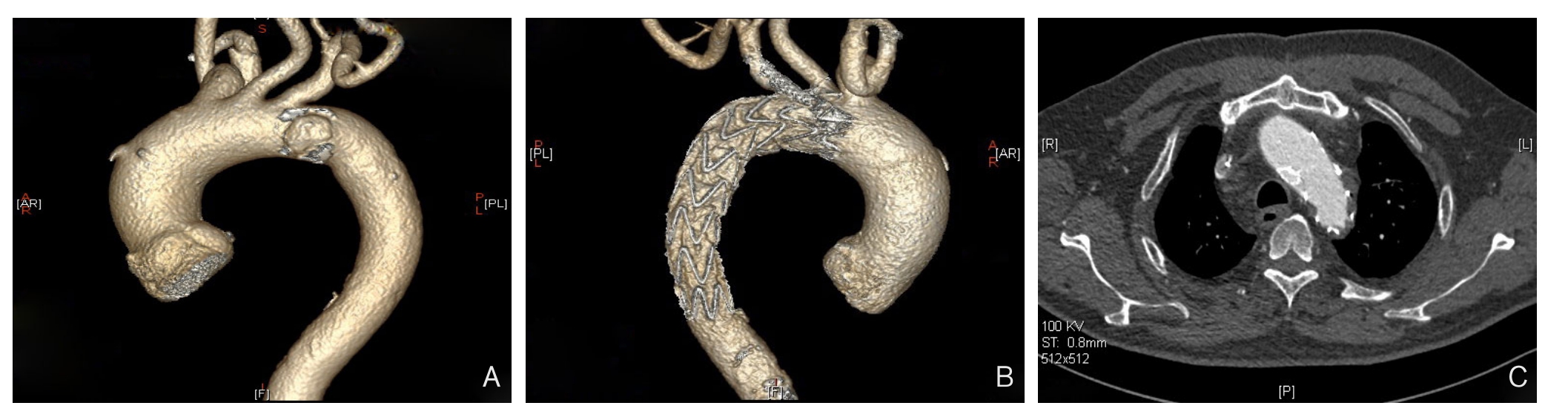
图1 “烟囱”支架植入术保留左锁骨下动脉 A:主动脉穿通性溃疡,缺乏近端锚定区;B:TEVAR结合“烟囱”技术重建左锁骨下动脉术后,锁骨下动脉通畅;C:左乳内动脉通畅,烟囱支架通畅
Figure 1 Chimney stent implantation for preserving the left subclavian artery A: Perforated ulcer in the aorta and the lack of an adequate landing zone; B: The patent left subclavian artery after reconstruction of the left subclavian artery by TEVAR combined with Chimney technique, C: Patent left internal mammary artery and Chimney stents
2.2 患者术后情况
手术成功率100%,左锁骨下动脉保留成功率100%。术后并发症包括I型内漏1例(1/9),随访3个月后消失。术后4个月因回旋支钙化狭窄进行PCI 1例(1/9)。所有患者均获得门诊或电话随访,随访时间6(4~7)个月,所有患者临床症状消失或明显减轻,生活质量改善,无随访期间死亡病例。
3 讨 论
随着我国人民生活水平的提高,饮食结构和生活方式的改变以及人均寿命的延长,高血压、高血脂、糖尿病、肥胖等危险因素日益流行,全身动脉粥样硬化性疾病已经成为常见病[5]。不同年龄段人群的冠心病发病率均呈现上升趋势,冠心病已逐步成为发展中国家主要的死亡原因之一[6]。同时,主动脉粥样硬化性病变如溃疡、动脉瘤等发病率和检出率也不断上升。因此,合并冠心病的主动脉疾病在临床上较为常见[7]。而当患者罹患严重冠心病需行冠状动脉旁路移植手术,同时合并主动脉弓降部病变需行TEVAR手术,作为一种较为复杂的合并疾患,在治疗上需要予以特殊考量。
随着介入技术的发展,越来越多的冠心病患者可接受微创的介入治疗[8],但对于左主干病变、三支病变等严重病例,大量循证医学证据表明,冠状动脉旁路移植手术仍然是其治疗的最佳手段[9]。目前,临床最常用的移植血管主要有左乳内动脉和大隐静脉。左乳内动脉属薄壁内脏小血管,管腔直径约为2~3 mm,血流速度快,不易产生内膜损伤,因此很少发生动脉粥样硬化;在冠状动脉旁路移植术中保留近端与左锁骨下动脉相连的血管蒂,术后其管腔所承受的压力、血流速度和血流量与在正常位置相似,避免了由于管壁承受的压力的变化引起的血管壁继发性改变;其内皮细胞分泌前列环素等血管舒缓因子,能扩张血管并根据生理需求调节血流量,前列环素还具有抗血小板聚积作用;而且左乳内动脉-前降支旁路移植术中只需1个吻合口,上述原因决定了左乳内动脉桥极高的远期通畅率。因此在多数情况下,左乳内动脉均作为前降支桥血管的最佳选择,以其良好的远期通畅率,长久保证左心室的血供。Kurlansky等[10-11]研究显示,应用乳内动脉行冠状动脉旁路移植手术的患者手术死亡比例明显降低。除前降支以外,其余冠脉靶血管的再血管化手术,一般采用大隐静脉[12-14]。大隐静脉有手术损伤小、易于获取等优点,但大隐静脉更易于发生粥样硬化而闭塞,远期通畅率显著低于动脉桥,如有研究证实大隐静脉桥与非致死性心肌梗死的风险增加相关[14-15]。
对于既往有冠状动脉旁路移植手术史并已行左乳内动脉-前降支旁路移植手术的患者,若合并主动脉弓降部疾患,尤其要注意TEVAR术中左锁骨下动脉的保护,绝不可覆盖,否则将带来致命性心肌梗死的风险。当近端锚定区不足时,可通过以下几点来避免左锁骨下动脉受损:⑴ 仔细判断主动脉弓降部疾患的危险程度及其手术指征,能保守治疗尽量保守治疗,尽可能避免手术操作;⑵ 通过严格控制支架释放瞬间的血压在低水平,由经验丰富的医生来实施手术等,尽可能精准释放主动脉覆膜支架,有助于精确锚定;⑶ 尽量避免左锁骨下动脉内部的操作,如“烟囱”支架的植入,因左锁骨下动脉腔内的操作也有可能导致术中左乳内动脉血供不稳定,理论上可能引发心脏突发事件。因此,本组4例左乳内动脉-前降支搭桥术后的患者,尽管锚定区仅为5~10 mm,均由经验丰富的术者直接实施了TEVAR手术,通过精准锚定实现了病变的隔绝和左锁骨下动脉的完整保留,其中支架型人工血管选取接近30%的放大倍率,以便使局部覆膜形成皱褶填充在主动脉溃疡內,可避免锚定区不足带来的内漏。但此操作具有较高风险,需要认真评估。
对于有严重冠心病,近期将接受冠状动脉旁路移植手术的患者,若合并主动脉弓降部疾患,也应注意TEVAR术中左锁骨下动脉的保护,尽量避免覆盖,为下一步的冠状动脉旁路移植手术保留左乳内动脉桥血管。本组5例此类患者,近端锚定区不足,2例通过精准锚定直接实施了TEVAR手术,保留了左乳内动脉,3例无法直接保留左锁骨下动脉的患者则通过“烟囱”技术重建了左锁骨下动脉的血供。根据本中心的随访结果,“烟囱”技术重建弓上动脉的通畅率令人满意[16-18]。
综上所述,对于已经接受左乳内动脉-冠脉前降支搭桥,或未来即将接受左乳内动脉-冠脉前降支搭桥手术的主动脉弓降部疾病患者,在实施TEVAR手术时采取综合措施保留左锁骨下动脉进而保留左乳内动脉极为重要,有望借此降低冠心病相关病死率,并提高生活质量。
参考文献
[1]Fattori R, Mineo G, Di Eusanio M.Acute type B aortic dissection:current management strategies[J].Curr Opin Cardiol, 2011,26(6):488–493.doi: 10.1097/HCO.0b013e32834a6fcc.
[2]JCS Joint Working Group.Guidelines for diagnosis and treatment of aortic aneurysm and aortic dissection (JCS 2011): digest version[J].Circ J, 2013, 77(3):789–828.
[3]Hajibandeh S, Hajibandeh S, Antoniou SA, et al.Metaanalysis of Left Subclavian Artery Coverage With and Without Revascularization in Thoracic Endovascular Aortic Repair[J].J Endovasc Ther, 2016, 23(4):634–641.doi: 10.1177/15266028166 51417.
[4]Loop FD, Lytle BW, Cosgrove DM, et al.Influence of the internal mammary artery graft on 10 year survival and other cardiac events[J].N Engl J Med, 1986, 314(1):1–6.
[5]李靓, 谢巍.我国动脉粥样硬化基础研究近三年进展[J].中国动脉硬化杂志, 2015, 23(11):1182–1188.Li L, Xie W.The Progress of the National Preclinical Research of Atherosclerosis in the Recent Three Years[J].Chinese Journal of Arteriosclerosis, 2015, 23(11):1182–1188.
[6]Gaziano TA, Bitton A, Anand S, et al.Growing epidemic of coronary heart disease in low- and middle-income countries[J].Curr Probl Cardiol, 2010, 35(2):72–115.doi: 10.1016/j.cpcardiol.2009.10.002.
[7]宋玮, 王爱萍, 闫文菊, 等.232例主动脉夹层相关危险因素分析[J].中国综合临床, 2016, 32(4):338–341.doi:10.3760/cma.j.issn.1008–6315.2016.04.015.Song W, Wang AP, Yan WJ, et al.Associated risk factors analysis of 232 cases of aortic dissection[J].Clinical Medicine of China, 2016,32(4):338–341.doi:10.3760/cma.j.issn.1008–6315.2016.04.015.
[8]Thomas MP, Bates ER.Update on primary PCI for patients with STEMI[J].Trends Cardiovasc Med, 2017, 27(2):95–102.doi:10.1016/j.tcm.2016.06.010.
[9]StephanWindecker, Kolh P, Alfonso F, et al.2014 ESC/EACTS guidelines on myocardial revascularization[J].Rev Esp Cardiol(Engl Ed), 2015, 68(2):144.doi: 10.1016/j.rec.2014.12.006.
[10]Kurlansky PA, Williams DB, Traad EA, et a1.Arterial grafting results in reduced operative mortality and enhanced long-term quality of life in octogenarians[J].Ann Thorac Surg, 2003,76(2):418–426.
[11]Subramanian S, Sabik JF 3rd, Houghtaling PL, et al.Decisionmaking for patients with patent left internal thoracic artery grafts to left anterior descending[J].Ann Thorac Surg, 87(5):1392–1398.doi:10.1016/j.athoracsur.2009.02.032.
[12]Tatoulis J.Giant leaps in surgical myocardial revascularization[J].Heart Lung Circ, 2011, 20(3):149–156.doi: 10.1016/j.hlc.2010.07.011.
[13]Hayward PA, Gordon IR, Hare DL, et a1.Comparable patencies of the radial artery and right internal thoracic artery or saphenous vein beyond 5 years: results from the Radial Artery Patency and Clinical Outcomes trial[J].J Thorac Cardiovase Surg, 2010, 139(1):60–65.doi: 10.1016/j.jtcvs.2009.09.043.
[14]Mehta RH, Honeycutt E, Peterson ED, et al.Impact of internal mammary artery conduit on long-term outcomes after percutaneous intervention of saphenous vein graft[J].Circulation, 2006, 114(1 Suppl):I396–401.
[15]Hillis LD, Smith PK, Anderson JL, et al.2011 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines[J].Circulation,2011, 124(23):e652–735.doi: 10.1161/CIR.0b013e31823c074e.
[16]舒畅, 罗明尧, 李全明, 等."烟囱"技术在累及主动脉弓部血管的动脉夹层腔内修复术中的应用[J].中国普通外科杂志, 2010,19(12):1266–1270.Shu C, Luo MY, Li QM, et al.Chimney grafts for endovascular repair of aortic dissection involving the aortic arch[J].Chinese Journal of General Surgery, 2010, 19(12):1266–1270.
[17]Shu C, Luo MY, Li QM, et al.Early results of left carotid chimney technique in endovascular repair of acute non-a-non-B aortic dissections[J].J Endovasc Ther, 2011, 18(4):477–484.doi:10.1583/11–3401.1.
[18]Liu H, Shu C, Li X, et al.Endovascular aortic repair combined with chimney technique in the treatment of stanford type B aortic dissection involving aortic arch[J].Ann Vasc Surg, 2015,29(4):758–763.doi: 10.1016/j.avsg.2014.12.004.
