乳糜胸是甲状腺癌颈淋巴结清扫术后的少见并发症,而双侧乳糜胸则更为罕见。双侧乳糜胸压迫肺部和纵膈可导致呼吸循环、代谢和免疫功能紊乱而危及生命。Stuart[1]在1907年首次报告颈淋巴清扫术后双侧乳糜胸,到目前为止国内外仍只有个案报道。现报告我院2000年1月至2016年10月共925例甲状腺癌颈部淋巴结清扫患者中2例双侧乳糜胸,并对相关文献进行复习。
1 临床资料
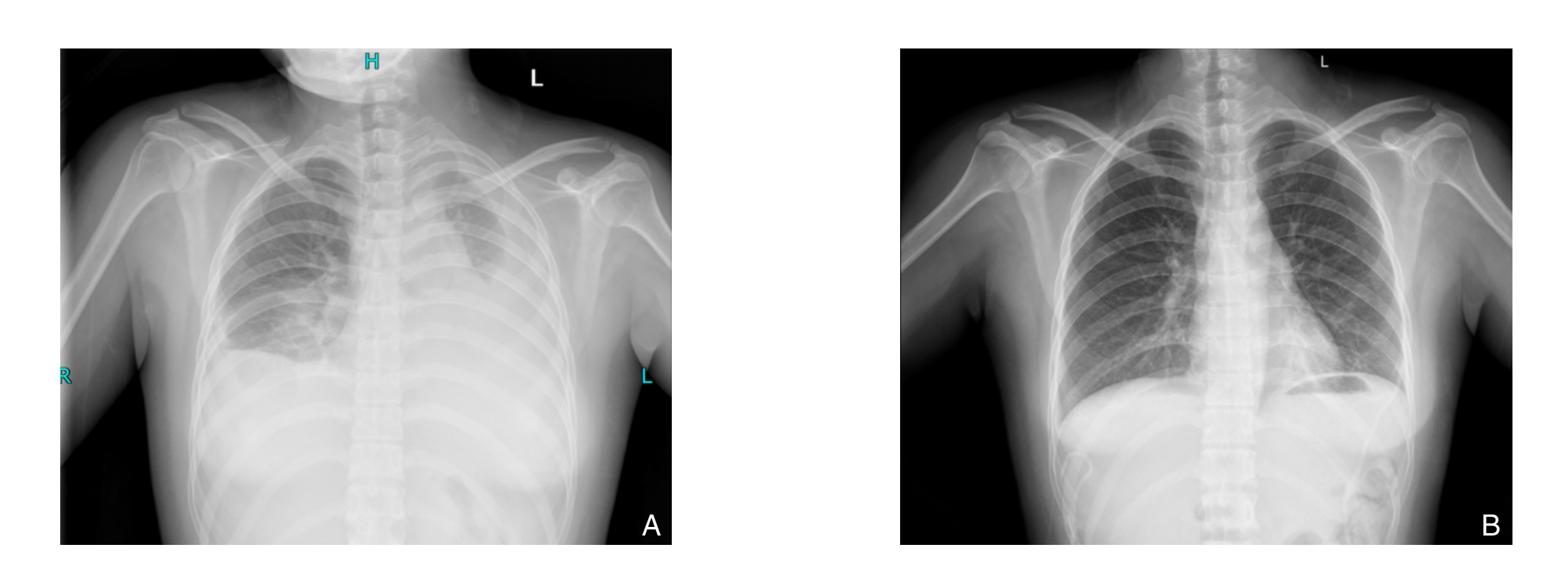
图1 患者1治疗前后胸片 A:术后第4天胸片可见双肺大片密度增高影,考虑为胸腔积液;B:术后14 d复查未见明显胸腔积液
Figure 1 Chest X-ray images of case 1 before and after treatment A: Massive high density shadows involving bilateral lungs in the X-ray image on postoperative day 4; B: No obvious thoracic fluid collections in the review X-ray image on postoperative day 14
患者1 女性,24岁。因发现甲状腺结节20余天入院。B超提示左侧甲状腺低回声结节并砂砾样钙化。术中经快速冷冻切片证实为甲状腺乳头状癌而行全甲状腺切除和左侧颈部淋巴结清扫术,术中仔细检查未发现淋巴渗漏,左侧颈部II、III、IV、V区淋巴结转移分别为5/5、1/8、6/9、0/2。术后颈部引流管无乳糜样淋巴液流出;第3天拨除颈部引流管;第4天出现气促和呼吸困难。经胸部X线检查为双侧胸腔积液,在超声引导下行双侧胸腔闭式引流出乳白色乳糜液约1 000 mL/每侧。予以禁食、胃肠外营养、奥曲肽(0.1 mg皮下注射,3次/d)等治疗后引流液逐渐减少、颜色变淡,减至300 mL时改低脂饮食。术后14 d未见明显引流液继续流出,复查胸部X线胸部无积液遂拨除胸部引流管出院。治疗前后胸部X线见图1.
患者2 女性,28岁。因发现甲状腺结节7个月入院。B超报告双侧甲状腺结节,左侧结节在甲状腺影像报告和数据系统(TI-RADS)分级中评为5类,双侧颈部淋巴结肿大考虑转移。经细针穿刺细胞学病理学检查诊断为甲状腺乳头状癌并双侧颈部淋巴结转移。遂行全甲状腺切除和双侧颈部淋巴结清扫术,术中静脉角处仔细结扎并探查未发现淋巴液渗漏,术后左侧颈部II、III、IV、V区淋巴结转移为5/12、3/6、4/9、0/2。术后第2天发现颈部引流管少许乳白色液体流出约10 mL,未予特殊处理而引流液减少至停止。术后第4天患者出现气促、呼吸困难,经胸部X线检查为双侧胸腔积液,在超声引导下穿刺双侧共引流出2 200 mL乳糜液。经禁食、奥曲肽等积极治疗后,左侧胸腔第2天引流减少,右侧胸腔第4天逐渐减少。术后8 d复查胸部X线无明显积液,术后第10天拨除引流管出院。治疗前后胸部X线见图2。

图2 患者2治疗前后胸片 A:术后第4天胸片可见双下肺大片致密影考虑双侧胸腔积液;B:术后10 d复查胸片胸腔积液明显减少
Figure 2 Chest X-ray images of case 1 before and after treatment A: Massive compact shades presenting in the inferior lungs on postoperative day 4 with consideration of bilateral hydrothorax; B: Significant reduction of fluid collections in the review X-ray image on postoperative day 10
2 文献复习与讨论
颈部淋巴结清扫的范围涉及包含胸导管等重要结构的肩胛舌骨肌锁骨三角,而胸导管的损伤是乳糜胸发生的主要原因。乳糜胸是颈部淋巴结清扫术后的少见并发症,发生率约为1%~2.5%[2]。双侧乳糜胸的发生更为少见,经搜索Pubmed数据库到目前为止收录相关文献报道仅29例(表1)。颈淋巴结清扫术后可出现双侧或单侧乳糜胸,发生率分别0.1%和0.2%[3]。我科925例颈部淋巴结清扫术后患者中仅出现2例发生率为0.22%,略高于文献报道。基于术后胸腔积液检查仅限于症状的患者,事实上乳糜胸的发生率可能被低估。乳糜胸可同时伴有或不伴有颈部淋巴漏,在查阅的27例患者其中10例同时伴有颈部切口乳糜胸[4]。本组患者中其中1例合并颈部乳糜漏,但量很少且于术后3 d拔出颈部引流管而自愈。乳糜胸常在术后3~4 d因气促、呼吸困难而被发现,如不及时处理常导致严重后果。Stuart[1]最先报道的3例颈淋巴清扫术后乳糜胸的患者均死于继发感染等并发症。胸部X线和B超检查可以提示诊断,胸腔穿刺引流出乳糜液可以明确诊断。本文报道2例均在术后4 d出现气促、呼吸困难而行胸片和B超检查,经穿刺引流出乳白色乳糜液证实。
表1 Pubmed文献报道的颈淋巴结清扫术后双侧乳糜胸病例资料
Table 1 Information of reported cases of bilateral chylothorax after neck dissection in Pubmed database
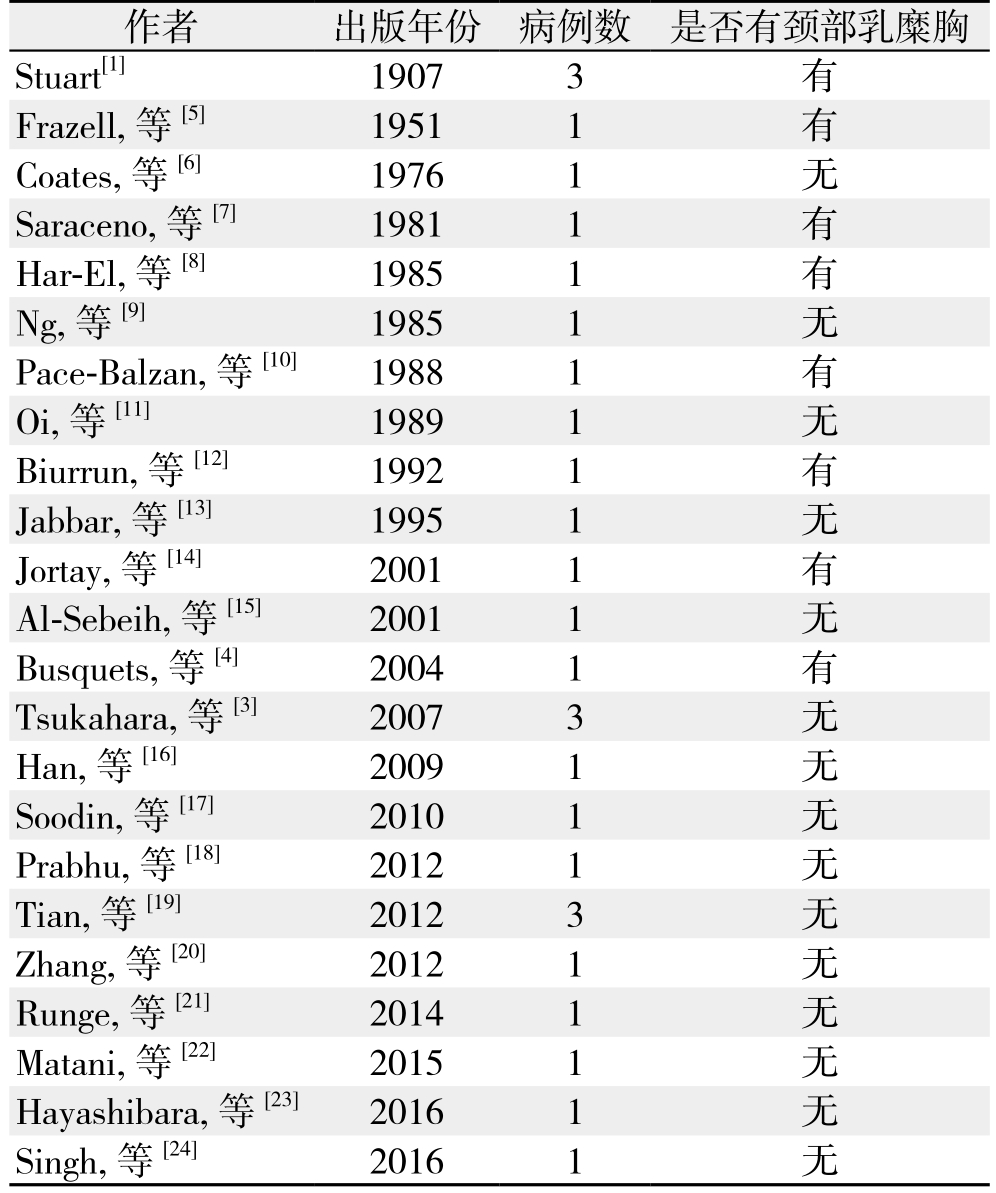
作者 出版年份 病例数 是否有颈部乳糜胸Stuart[1] 1907 3 有Frazell, 等[5] 1951 1 有Coates, 等[6] 1976 1 无Saraceno, 等[7] 1981 1 有Har-El, 等[8] 1985 1 有Ng, 等[9] 1985 1 无Pace-Balzan, 等[10] 1988 1 有Oi, 等[11] 1989 1 无Biurrun, 等[12] 1992 1 有Jabbar, 等[13] 1995 1 无Jortay, 等[14] 2001 1 有Al-Sebeih, 等[15] 2001 1 无Busquets, 等[4] 2004 1 有Tsukahara, 等[3] 2007 3 无Han, 等[16] 2009 1 无Soodin, 等[17] 2010 1 无Prabhu, 等[18] 2012 1 无Tian,等[19] 2012 3 无Zhang, 等[20] 2012 1 无Runge, 等[21] 2014 1 无Matani, 等[22] 2015 1 无Hayashibara, 等[23] 2016 1 无Singh, 等[24] 2016 1 无
颈部淋巴结清扫术后乳发生糜胸的机制尚不清楚,目前存在两种推断。其中一种推测认为颈部存在活动性淋巴漏,乳糜液直接从颈根部直接流入纵膈并压力的作用下经胸膜渗入胸腔内。这种观念在因同时存在颈部乳糜胸的患者中而看似合理。另外一种观念认为是术中胸导管被结扎,由于胸导管的压力急剧上升和在胸腔内负压作用下乳糜液渗入胸腔内从而形成乳糜胸。本组报道的2例中1例颈部仅出现少许乳糜漏且未影响引流管的拨除和伤口的愈合。此外从总结文献报道的29例患者资料来看,近10余年来报道的病例均未同时出现颈部活动性淋巴漏。有报道[3,25]甲状腺癌行颈淋巴清扫术后发生双侧乳糜胸患者在术中及关闭切口前均进行破坏性挤压试验及胸腔加压,均未发现颈部乳糜漏。因此,笔者推测后一种机制可能是双侧乳糜胸形成的主要原因。
乳糜胸的治疗主要以保守治疗为主,包括及时充分引流、低脂饮食或禁食、胃肠外营养、预防感染和水电解质紊乱。胸腔闭式引流有利于迅速解除压迫、缓解呼吸困难等症状,同时有利于观察引流液性状和流量以便于采取进一步的治疗措施。禁食或低脂饮食、胃肠外营养能降低胃肠道的负担,减少乳糜的形成。奥曲肽是一种人工合成的多肽可作用于淋巴管上的特殊受体减少胃肠道蠕动和淋巴液的生成,从而达到治疗乳糜胸的目的[23]。本组2例患者采用上述包括奥曲肽的保守治疗后,胸腔乳糜液的颜色逐渐变淡且引流量逐渐减少。如果经过积极的保守治疗1~2周后引流量没有明显减少且持续在1 L/d以上,应采取手术治疗如开胸或胸腔镜下胸导管结扎术。Polistena等[2]认为胸导管结扎可能是保守治疗无效后治疗乳糜胸的唯一方法。相对于开胸手术,胸腔镜具有创伤小、恢复快等特点的安全有效方法[26]。经文献复习除最早由Stuart等[1]报道的3例因感染等原因死亡外,其他病例均未出现严重后果,这可能是早期对乳糜漏包括乳糜胸的认识不足和缺乏术后有效处理措施等造成。本组2例患者经积极的保守治疗,术后10~14 d经顺利出院而未发生严重后果。
总之,甲状腺癌颈淋巴清扫术后乳糜胸是一种罕见的并发症。避免术中胸导管的损伤和早期发现是关键,一旦诊断经积极保守治疗和胸导管结扎等治疗后一般不会发生严重后果。
参考文献
[1] Stuart WJ. Operative injury of the thoracic duct in the neck[J].Edinb Med J, 1907, 22:301–306.
[2] Polistena A, Vannucci J, Monacelli M, et al. Thoracic duct lesions in thyroid surgery: An update on diagnosis, treatment and prevention based on a cohort study[J]. Int J Surg, 2016, 28(Suppl 1): S33–37.doi: 10.1016/j.ijsu.2015.05.058.
[3] Tsukahara K, Kawabata K, Mitani H, et al. Three cases of bilateral chylothorax developing after neck dissection[J]. Auris Nasus Larynx, 2007, 34(4):573–576.
[4] Busquets JM, Rullan PJ, Trinidad-Pinedo J. Bilateral chylothorax after neck dissection[J]. Otolaryngol Head Neck Surg, 2004,130(4):492–495.
[5] Frazell EL, Harrold CC Jr, Rasmussen L. Bilateral chylothorax; an unusual complication of radical neck dissection with recovery[J].Ann Surg, 1951, 134(1):135–137.
[6] Coates HL, DeSanto LW. Bilateral chylothorax as a complication of radical neck dissection[J]. J Laryngol Otol, 1976, 90(10):967–970.
[7] Saraceno CA, Farrior RT. Bilateral chylothorax. Rare complication of neck dissection[J]. Arch Otolaryngol, 1981, 107(8):497–499.
[8] Har-El G, Segal K, Sidi J. Bilateral chylothorax complicating radical neck dissection: report of a case with no concurrent external chylous leakage[J]. Head Neck Surg, 1985, 7(3):225–230.
[9] Ng RS, Kerbavaz RJ, Hilsinger RL Jr. Bilateral chylothorax from radical neck dissection[J]. Otolaryngol Head Neck Surg, 1985,93(6):814–817.
[10] Pace-Balzan A, Moriarty B. Bilateral chylothorax following left radical neck dissection (case report)[J]. J Laryngol Otol, 1988,102(3):288–290.
[11] Oi K, Haraguchi N, Machida S, et al. Dyspnea resulting from accumulation of pleural effusion after radical neck dissection. A case report[J]. Oral Surg Oral Med Oral Pathol, 1989, 67(3):258–261.
[12] Biurrun O, Sabater F, Traserra J. Bilateral chylothorax after radical neck dissection. Apropos of a case[J]. Rev Laryngol Otol Rhinol(Bord), 1992, 113(2):111–113.
[13] Jabbar AS, al-Abdulkareem A. Bilateral chylothorax following neck dissection[J]. Head Neck, 1995, 17(1):69–72.
[14] Jortay A, Bisschop P. Bilateral chylothorax after left radical neck dissection[J]. Acta Otorhinolaryngol Belg, 2001, 55(4):285–289.
[15] Al-Sebeih K, Sadeghi N, Al-Dhahri S. Bilateral chylothorax following neck dissection: a new method of treatment[J]. Ann Otol Rhinol Laryngol, 2001, 110(4):381–384.
[16] Han C, Guo L, Wang KJ, et al. Bilateral chylothorax following neck dissection for thyroid cancer[J]. Int J Oral Maxillofac Surg, 2009,38(10):1119–1122. doi: 10.1016/j.ijom.2009.04.018.
[17] Soodin D, Singh P, Irani D, et al. Bilateral chylothorax following left sided modified radical neck dissection[J]. Ceylon Med J, 2010,55(4):126–127.
[18] Prabhu V, Passant C. Left-sided neck dissection and chylothorax:a rare complication and its management[J]. J Laryngol Otol, 2012,126(6):648–650. doi: 10.1017/S002221511200062X.
[19] Tian W, Li ZY, Wang P, et al. Chylothorax after neck dissection for thyroid carcinomas: report of three cases[J]. Surg Today, 2012,42(1):89–92. doi: 10.1007/s00595–011–0015–6.
[20] Zhang H, Dziegielewski PT, Romanovsky A, et al. Bilateral chylothorax following neck dissection: case report and systematic review of the literature[J]. J Otolaryngol Head Neck Surg, 2012,41(4):E26–30.
[21] Runge T, Borbély Y, Candinas D, et al. Bilateral chylothorax following neck dissection: a case report[J]. BMC Res Notes, 2014,7:311. doi: 10.1186/1756–0500–7–311.
[22] Matani S, Pierce JR Jr. Spilt Milk: An Unusual Cause of Bilateral Chylothorax[J]. J Investig Med High Impact Case Rep, 2015,3(2):2324709615583877. doi: 10.1177/2324709615583877.
[23] Hayashibara N, Ogawa T, Tsuji E, et al. Efficacy of octreotide against chylothorax following lateral neck dissection for thyroid cancer: A case report[J]. Int J Surg Case Rep, 2016, 21:107–110.doi: 10.1016/j.ijscr.2016.02.025.
[24] Singh R, Krishnan S, George NA, et al. Bilateral Chylothorax Following Neck Dissection: Case Report & Review of Literature[J].Indian J Surg Oncol, 2016, 7(1):115–118. doi: 10.1007/s13193–015–0445–5.
[25] 吴贤江, 李健君, 戴磊, 等. 甲状腺癌患者行颈淋巴清扫术后并发乳糜胸11例临床分析[J]. 中华危重症医学杂志:电子版, 2015,8(4):256–257. doi:10.3877/cma.j.issn.1674–6880.2015.04.011.Wu XJ, Li JJ, Dai L, et al. Chylothorax in thyroid cancer patients after neck dissection: a clinical analysis of 11 cases[J]. Chinese Journal of Critical Care Medicine: Electronic Edition, 2015,8(4):256–257. doi:10.3877/cma.j.issn.1674–6880.2015.04.011.
[26] Ikeda Y. Thoracoscopic management of cervical thoracic duct injuries after thyroidectomy with lymphadenectomy[J]. Asian J Endosc Surg, 2014, 7(1):82–84. doi: 10.1111/ases.12075.
