我国胆囊结石患者中约10%~15%合并胆总管结石,其发病率随年龄增加而升高。随着腹腔镜技术和内镜设备的不断进步,越来越多的胆总管结石可以通过腹腔镜胆总管探查术(laparoscopic common bile duct exploration,LCBDE)进行处理[1-5]。鉴于LCBDE术后留置T管给患者带来的诸多不便,以及T管的拔除可能导致相关并发症,国内外学者[6-10]先后开展了LCBDE一期缝合术,结果显示不放置T管并未增加术后并发症。随着我国老年人口比例的不断攀升,其胆总管结石的发病率也逐渐增加。但老年患者常合并高血压、糖尿病、冠心病、慢性支气管炎、脑梗死等疾病,增加了手术风险,同时CO2气腹压力也对老年患者心肺功能和循环产生一定影响,因此老年患者能否采用该术式需要进一步探讨[11-14]。2012年12月—2016年12月,我院对146例胆囊结石合并胆总管结石患者施行LCBDE一期缝合术,其中老年患者61例,非老年患者85例,现将临床资料报告如下。
1 资料与方法
1.1 临床资料
入组患者146例,年龄为17~93岁,其中老年患者(≥65岁)61例,平均年龄74.02岁;男30例,女31例;体质量指数(BMI)平均25.3;既往腹部手术史5例(胃溃疡穿孔修补1例、开腹阑尾切除2例、剖宫产1例、子宫切除1例),伴有高血压24例、糖尿病13例、冠心病5例。非老年患者(<65岁)85例,平均年龄50.25岁;男41例,女44例;BMI平均24.8;既往腹部手术史13例(剖宫产8例、子宫切除3例、开腹阑尾切除2例),伴有高血压14例、糖尿病4例、冠心病2例(表1)。所有患者术前均行MRCP或CT等检查证实为胆总管结石。
表1 两组患者一般资料比较
Table 1 Comparison of general data of the two groups of patients
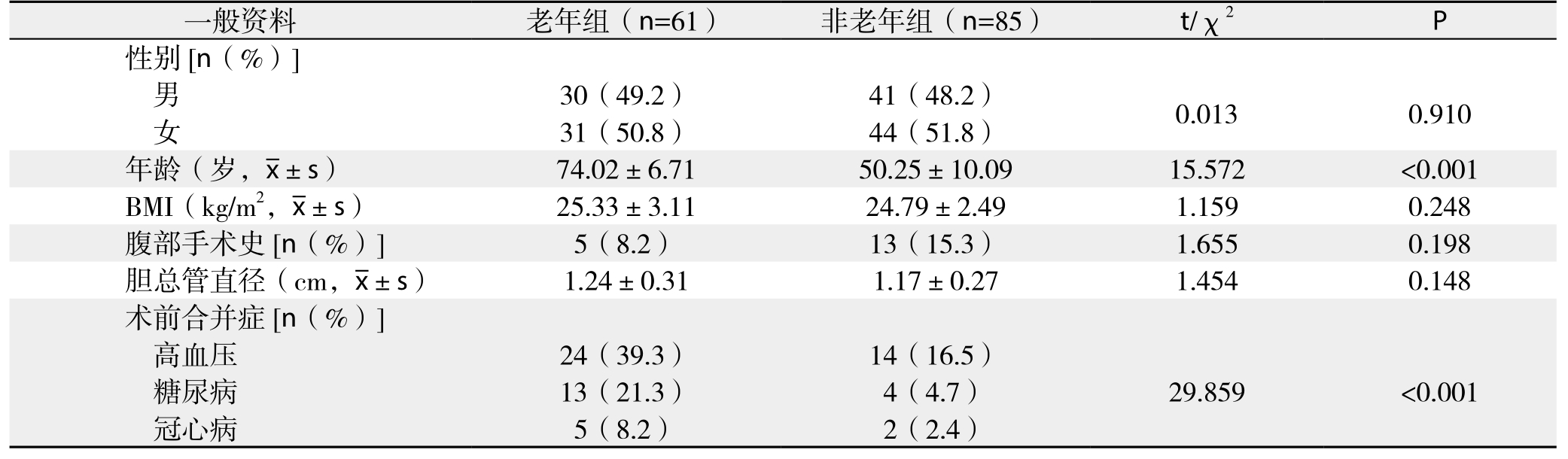
一般资料 老年组(n=61) 非老年组(n=85) t/χ2 P性别[n(%)]男30(49.2) 41(48.2) 0.013 0.910女31(50.8) 44(51.8)年龄(岁,x±s) 74.02±6.71 50.25±10.09 15.572 <0.001 BMI(kg/m2,x±s) 25.33±3.11 24.79±2.49 1.159 0.248腹部手术史[n(%)] 5(8.2) 13(15.3) 1.655 0.198胆总管直径(cm,x±s) 1.24±0.31 1.17±0.27 1.454 0.148术前合并症[n(%)]高血压 24(39.3) 14(16.5)糖尿病 13(21.3) 4(4.7) 29.859 <0.001冠心病 5(8.2) 2(2.4)
1.2 手术方法
气管插管静脉复合麻醉,≥65岁患者气腹压力维持在10~12 mmHg(1 mmHg=0.133 kPa)或<65岁患者12~14 mmHg左右,四孔法进行手术。腹腔探查后解剖胆囊三角,距胆总管0.5 cm夹闭胆囊管暂不切断,既防止小结石被挤入胆总管,也便于术中牵引。显露胆总管,依据结石大小纵行切开胆总管前壁0.5~1.5 cm。将冲洗器或者胆道镜置入胆总管加压冲洗可冲出部分细小结石,然后置入纤维胆道镜探查,发现结石则置入Cook网篮取出。如取石困难,可采用取石钳、液电碎石等方法取石。反复确认无结石残留,胆管下端通畅无狭窄后,4-0 Vicryl线连续缝合胆总管壁,针距和边距约为2.0~2.5 mm,两端缝合均应超过切口2.0 mm。缝合完毕置入小纱布蘸拭切口创面,确认无胆汁渗漏后,于右肝外缘放置引流管1根,自肋缘下锁骨中线Trocar孔引出固定。缓慢排净CO2气腹,确认引流管无弯折盘曲后再缝合固定。
1.3 术后处理
术后第2天给予流食,术后前3 d常规予以抗生素预防或治疗感染。腹腔引流量连续2 d少于20 mL/d,患者无腹膜炎表现,即拔除引流管。术后通过门诊复查和电话方式随访,术后1个月复查B超,此后每半年复查1次,至术后3年。
1.4 统计学处理
应用SPSS 19.0软件进行统计学处理,计量资料采用均数±标准差( ±s)的描述,组间比较采用t检验,计数资料以例(%)表示,采用χ2检验,P<0.05为差异有统计学意义。
±s)的描述,组间比较采用t检验,计数资料以例(%)表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结 果
2.1 术中与术后情况
146例患者行腹腔镜胆总管探查一期缝合手术均获成功,无中转开腹。老年组与非老年组患者的手术时间、术中出血量、胆总管结石数量差异无统计学意义(均P>0.05);老年组术后腹腔引流时间、胃肠功能恢复时间、术后下床时间、术后住院时间等指标均明显长于非老年组,差异有统计学意义(均P<0.05)(表2)。
表2 两组患者术中与术后资料比较( ±s)
±s)
Table 2 Comparison of intra- and postoperative data between the two groups of patients  ±s)
±s)
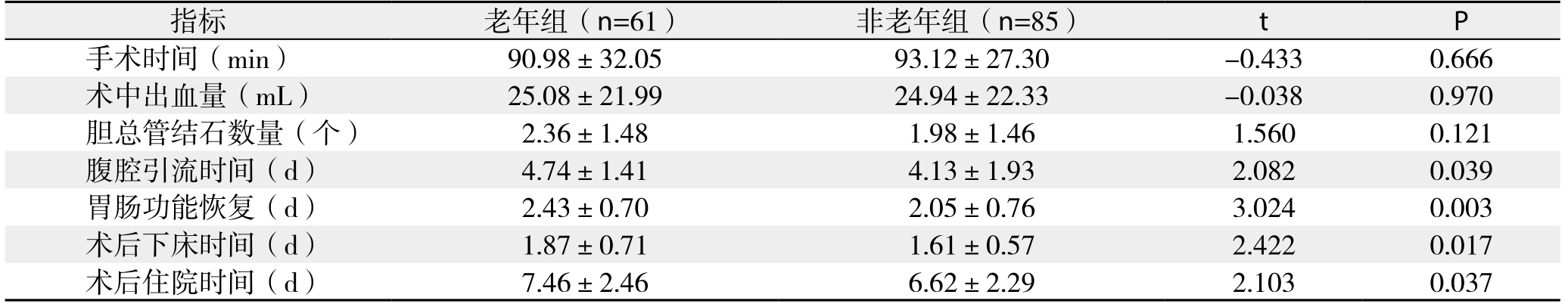
指标 老年组(n=61) 非老年组(n=85) t P手术时间(min) 90.98±32.05 93.12±27.30 -0.433 0.666术中出血量(mL) 25.08±21.99 24.94±22.33 -0.038 0.970胆总管结石数量(个) 2.36±1.48 1.98±1.46 1.560 0.121腹腔引流时间(d) 4.74±1.41 4.13±1.93 2.082 0.039胃肠功能恢复(d) 2.43±0.70 2.05±0.76 3.024 0.003术后下床时间(d) 1.87±0.71 1.61±0.57 2.422 0.017术后住院时间(d) 7.46±2.46 6.62±2.29 2.103 0.037
2.2 术后并发症及随访情况
两组患者术后均未发生急性胰腺炎、腹腔感染、切口感染等严重并发症。老年组和非老年组分别有1例和2例患者出现术后腹腔出血,出血量合计分别为83、55、120 mL,3例均经过静脉给予止血药物治疗3~5 d后痊愈。本研究146例患者发生胆汁漏14例(9.6%),老年组发生胆汁漏6例(9.8%),每天引流量为30~150 mL,其中5例持续腹腔引流7~12 d后痊愈,另1例为术后第4天引流液突然消失伴腹膜炎表现,急诊CT见肝周、脾周、盆腔积液,行腹腔镜探查发现胆总管第1针缝合间距过大,胆汁渗漏明显,而引流管因网膜堵塞导致引流不畅,冲洗并吸净腹腔后4-0 Vicryl线“8”字缝合修补切口,并重新留置腹腔引流管,第2次术后5 d出院。非老年组发生术后胆汁漏8例(9.4%),每天引流量为20~110 mL,持续腹腔引流6~11 d后痊愈。术后随访6~36个月,两组患者残余结石率、结石复发率均无统计学差异(P>0.05),两组患者术后未发生胆总管狭窄(表3)。另外,老年组患者术后有1例发生肺部感染,经抗感染、雾化吸入等治疗5 d后好转,另1例发生心功能不全,经控制输液速度、利尿等治疗1 d后好转。
表3 两组患者术后并发症与随访资料比较[n(%)]
Table 3 Comparison of postoperative complications and follow-up data between the two groups [n (%)]
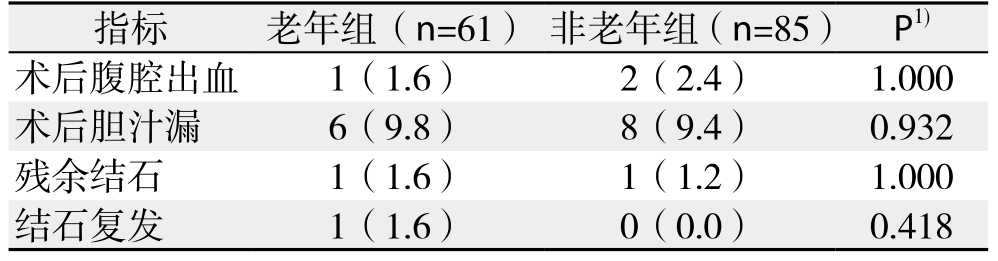
注:1)采用Fisher确切概率法
Note: 1) using Fisher’s exact test
指标 老年组(n=61) 非老年组(n=85) P1)术后腹腔出血 1(1.6) 2(2.4) 1.000术后胆汁漏 6(9.8) 8(9.4) 0.932残余结石 1(1.6) 1(1.2) 1.000结石复发 1(1.6) 0(0.0) 0.418
3 讨 论
3.1 老年胆总管结石患者的微创治疗选择
随着人口老龄化程度的日益加重,老年胆囊结石合并胆总管结石患者逐年增多,成为老年人的常见疾病。老年患者往往伴有合并症,手术耐受性差,手术风险较高[5,11-14]。传统开腹手术存在创伤大、恢复慢、并发症多等缺点,其治疗方式逐渐向微创化趋势发展。但目前的微创治疗方法也各自有其缺点:如EST存在出血、胰腺炎、肠穿孔等风险,也破坏了Oddi括约肌的结构和功能,同时EST术后还需要二期行腹腔镜胆囊切除[15-18];腹腔镜经胆囊管取石术有一定优势,但技术操作更为复杂,且受到结石数量、大小、结石位置、胆囊管解剖变异等限制[19-20]。LCBDE术后留置T管存在胆汁大量丢失、T管携带不便、T管意外脱出引起腹膜炎等弊端[21]。而LCBDE一期缝合则具有明显的优势,本研究结果显示,尽管老年患者的术前合并症明显多于非老年患者,但手术时间、术中出血量、术后胆汁漏、术后腹腔出血、残余结石、结石复发率等指标与后者无统计学差异,老年患者采用LCBDE一期缝合术式同样安全、可行。
3.2 老年患者LCBDE一期缝合适应证
目前尚无统一的老年患者LCBDE一期缝合适应证标准。结合前期的临床实践,我们认为应遵循的适应证为:⑴ 术前MRCP或CT证实为胆总管结石,无肝内胆管结石;⑵ 胆总管直径≥0.8 cm;⑶ 胆总管下端通畅,Oddi括约肌功能良好、远端无狭窄;⑷ 既往无胆道手术史;⑸ ASA分级标准3级以下。排除标准为:合并重症胆管炎、急性胰腺炎或胆道恶性肿瘤。
3.3 老年患者围手术期处理
老年患者机体代偿能力差、合并症多,手术风险明显增加,术后恢复较慢。因此积极进行围手术期处理至关重要[11-14]。高血压患者应该将血压控制在160/90 mmHg以下,手术当日清晨口服降压药;2型糖尿病患者空腹血糖控制在8.0 mmol/L以下;对肺功能差的患者术前进行7 d以上吹气训练,并鼓励患者咳嗽咳痰,每日2~3次雾化吸入;长期口服氯吡格雷、阿司匹林等抗凝药物患者,术前至少停药7 d;对于肾功能不全患者,除术前避免使用肾损害药物、纠正水电解质紊乱以外,术中、术后要注意控制输液量和输液速度,避免肾脏低灌注损伤,并动态监测肾功能和电解质。对于多个重要脏器功能均较差患者,术前应组织多学科病例讨论,共同制订围手术期治疗方案。另外术中气腹压力应降低至10~12 mmHg,减少气腹压力对患者心、肺功能和血流动力学的影响,确保手术安全。
3.4 术后胆汁漏的的预防和处理
胆汁漏是LCBDE术后的主要并发症,文献报道发生率为1.7%~25.3%[4,22-25]。本研究146例患者发生胆汁漏14例(9.6%),其中13例经过持续腹腔引流痊愈,仅1例72岁老年患者行二次腹腔镜修补。此病例再次手术是胆总管第1针缝合间距过大导致胆汁漏,而腹腔引流管又被网膜包裹造成引流不畅两个因素叠加所致。对此笔者有几点体会:⑴ 在缝合胆总管切口上端第一针时,应超过切口部位2 mm,这样在缝合过程中即使被反复牵引,也不易出现缝线移位造成缝合间距过大出现胆汁漏;⑵ 推荐连续缝合,既能减少反复打结和剪线步骤提高缝合效率,又能保证切口张力均匀适中,减少胆汁渗漏;⑶ 缝合时要疏密均匀,边距和针距应保持在2.0~2.5 mm,下端缝合也应该超过切口2.0 mm;⑷ 对于部分胆管壁菲薄的患者,缝合后往往发生针孔处胆汁渗漏,而反复进针和牵拉也容易造成针孔切割,加重胆汁渗漏,对此我们在连续缝合后,再间断缝合胆管壁浆膜层,以可以减少胆汁漏的发生;⑸ 胆总管下端通畅是减少胆汁漏的前提,缝合前应在胆道镜下反复确认无结石残留,对于可疑十二指肠乳头结石嵌顿者,可静脉给予阿托品5~10 mg舒张Oddi括约肌以便于观察;⑹ 通畅的腹腔引流能够降低LCBDE一期缝合术后二次手术的风险,建议采用有内支撑的引流管,引流管应放置在右肝外侧缘,可以减少引流管被大网膜包裹堵塞的可能性。
本研究结果显示,与非老年患者相比,老年胆总管结石患者行LCBDE一期缝合同样安全有效,符合加速康复外科的理念[26]。在准确把握手术指证的前提下,LCBDE一期缝合可作为老年胆总管结石患者优先选择的术式。
参考文献
[1] Chan DS, Jain PA, Khalifa A, et al. Laparoscopic common bile duct exploration[J]. Br J Surg, 2014, 101(11):1448–1452. doi: 10.1002/bjs.9604.
[2] 张乐, 白月奎, 欧云菘, 等. 腹腔镜胆囊切除胆道探查术治疗胆囊结石合并胆总管结石的临床观察[J]. 中国普通外科杂志, 2014,23(8):1141–1143. doi:10.7659/j.issn.1005–6947.2014.08.028.Zhang L, Bai YK, Ou YS, et al. Clinical study of laparoscopic common bile duct exploration for cholecystolithiasis combined with choledocholithiasis[J]. Chinese Journal of General Surgery, 2014,23(8):1141–1143. doi:10.7659/j.issn.1005–6947.2014.08.028.
[3] Gupta N. Role of laparoscopic common bile duct exploration in the management of choledocholithiasis[J]. World J Gastrointest Surg,2016, 8(5):376–381. doi: 10.4240/wjgs.v8.i5.376.
[4] Lee HM, Min SK, Lee HK. Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis: 15-year experience from a single center[J]. Ann Surg Treat Res, 2014, 86(1):l-6. doi: 10.4174/astr.2014.86.1.1.
[5] Zheng C, Huang Y, Xie E, et al. Laparoscopic common bile duct exploration: a safe and definitive treatment for elderly patients[J].Surg Endosc, 2017, 31(6):2541–2547. doi: 10.1007/s00464–016–5257–3.
[6] 刘东斌, 刘家峰, 徐大华, 等. 腹腔镜胆总管探查一期缝合术并发症及治疗策略[J]. 腹腔镜外科杂志, 2015, 20(11):855–858. doi:10.13499/j.cnki.fqjwkzz.2015.11.855.Liu DB, Liu JF, Xu DH, et al. The complications and treatment strategies for laparoscopic common bile duct exploration and primary suture[J]. Journal of Laparoscopic Surgery, 2015,20(11):855–858. doi: 10.13499/j.cnki.fqjwkzz.2015.11.855.
[7] 徐红星, 徐海宾, 顾玉青, 等. 腹腔镜胆总管探查术后一期缝合与T管引流的临床研究[J]. 中国普外基础与临床杂志, 2015,22(10):1254–1256.Xu HX, Xu HB, Gu YQ, et al. Clinical comparison between laparoscopic common bile duct exploration with primary closure and T-tube drainage[J]. Chinese Journal of Bases and Clinics In General Surgery, 2015, 22(10):1254–1256.
[8] Dong ZT, Wu GZ, Luo KL, et al. Primary closure after laparoscopic common bile duct exploration versus T-tube[J]. J Surg Res, 2014,189(2):249–254. doi: 10.1016/j.jss.2014.03.055.
[9] Wen SQ, Hu QH, Wan M, et al. Appropriate Patient Selection Is Essential for the Success of Primary Closure After Laparoscopic Common Bile Duct Exploration[J]. Dig Dis Sci, 2017, 62(5):1321–1326. doi: 10.1007/s10620–017–4507–0.
[10] Podda M, Polignano FM, Luhmann A, et al. Systematic review with meta-analysis of studies comparing primary duct closure and T-tube drainage after laparoscopic common bile duct exploration for choledocholithiasis[J]. Surg Endosc, 2016, 30(3):845–861. doi:10.1007/s00464–015–4303–x.
[11] 刘立川, 张峻, 刘伟. 腹腔镜胆总管探查术治疗老年胆总管结石[J]. 中国普通外科杂志, 2014, 23(8):1154–1156. doi:10.7659/j.issn.1005–6947.2014.08.033.Liu LC, Zhang J, Liu W. Laparoscopic common bile duct exploration for elderly patients with common bile duct stones[J].Chinese Journal of General Surgery, 2014, 23(8):1154–1156.doi:10.7659/j.issn.1005–6947.2014.08.033.
[12] 梁阔, 刘东斌, 刘家峰, 等. 腹腔镜胆总管探查一期缝合在老年胆总管结石病人中的应用[J]. 首都医科大学学报, 2017, 38(1):78–81. doi:10.3969/j.issn.1006–7795.2017.01.016.Liang K, Liu DB, Liu JF, et al. Application of laparoscopic common bile duct exploration with primary closure in treatment of choledocholithiasis in elderly patients[J]. Journal of Capital Medical University, 2017, 38(1):78–81. doi:10.3969/j.issn.1006–7795.2017.01.016.
[13] 刘东斌, 刘家峰, 徐大华, 等. 老年胆石症患者腹腔镜胆总管切开取石一期缝合35例分析[J]. 实用老年医学, 2013, 27(10):847–849.doi: 10.3969/j.issn.1003–9198.2013.10.017.Liu DB, Liu JF, Xu DH, et al. Laparoscopic common bile duct exploration and primary suture for the treatment of thirty-five elderly patients with common duct stones[J]. Practical Geriatrics,2013, 27(10):847–849. doi: 10.3969/j.issn.1003–9198.2013.10.017.
[14] 王中魁, 赵海鹰, 刘金钢, 等. 老年人胆囊结石合并胆总管结石术式选择探讨[J]. 中国实用外科杂志, 2015, 35(4):448–450.Wang ZK, Zhao HY, Liu JG, et al. Comparison of operative methods for older patients with concomitant cholelithiasis and choledocholithiasis: a report of 60 patients[J]. Chinese Journal of Practical Surgery, 2015, 35(4):448–450.
[15] Oliveira-Cunha M, Dennison AR, Garcea G. Late Complications After Endoscopic Sphincterotomy[J]. Surg Laparosc Endosc Percutan Tech, 2016, 26(1):1–5. doi: 10.1097/SLE.0000000000000226.
[16] Koc B, Karahan S, Adas G, et al. Comparison of laparoscopic common bile duct exploration and endoscopic retrogradecholangiopancreatography plus laparoscopic cholecystectomy for choledocholithiasis: a prospective randomized study[J]. Am J Surg,2013, 206(4):457–463. doi: 10.1016/j.amjsurg.2013.02.004.
[17] 李宇, 郝杰, 孙昊, 等. 一期腹腔镜胆囊切除联合胆总管探查取石与分期内镜取石和腹腔镜胆囊切除术治疗胆囊结石合并胆总管结石的比较[J]. 中国普通外科杂志, 2016, 25(2):202–208.doi:10.3978/j.issn.1005–6947.2016.02.008.Li Y, Hao J, Sun H, et al. One-staged laparoscopic cholecystectomy and common bile duct exploration versus two-staged endoscopic stone extraction followed by laparoscopic cholecystectomy for concomitant cholecystolithiasis and choledocholithiasis[J]. Chinese Journal of General Surgery, 2016, 25(2):202–208. doi:10.3978/j.issn.1005–6947.2016.02.008.
[18] 殷晓煜. 胆道外科手术中Oddi括约肌保护的共识与争议[J]. 中国实用外科杂志, 2015, 35(1):46–48.Duan XY. Consensus and controversies on protection of sphincter of Oddi during biliary surgery[J]. Chinese Journal of Practical Surgery, 2015, 35(1):46–48.
[19] 张淼, 谈永飞. 腹腔镜下经胆囊管胆总管探查术与胆总管探查并一期缝合术治疗胆总管结石的对比研究[J]. 中国普通外科杂志,2017, 26(2):151–156. doi:10.3978/j.issn.1005–6947.2017.02.004.Zhang M, Tan YF. Comparison of laparoscopic transcystic common bile duct exploration and laparoscopic common bile duct exploration with primary suture for common bile duct stones[J].Chinese Journal of General Surgery, 2017, 26(2):151–156.doi:10.3978/j.issn.1005–6947.2017.02.004.
[20] 朱杰高, 张忠涛, 韩威, 等. 经胆囊管途径探查取石失败后的应对策略[J]. 中华肝胆外科杂志, 2014, 20(3):224–226. doi:10.3760/cma.j.issn.1007–8118.2014.03.019.Zhu JG, Zhang ZT, Han W, et al. Countermeasures for failure in exploration and stone extraction via gallbladder approach[J].Chinese Journal of Hepatobiliary Surgery, 2014, 20(3):224–226.doi:10.3760/cma.j.issn.1007–8118.2014.03.019.
[21] 郑志鹏, 何军明, 钟小生, 等. 腹腔镜胆总管探查术后拔T管胆瘘的防治[J]. 中国普通外科杂志, 2013, 22(2):252–254. doi:10.7659/j.issn.1005–6947.2013.02.029.Zheng ZP, He JM, Zhong ZS, et al. Prophylaxis and treatment of bile leakage after T-tube drainage of laparoscopic common bile duct exploration[J]. Chinese Journal of General Surgery, 2013,22(2):252–254. doi:10.7659/j.issn.1005–6947.2013.02.029.
[22] 冯林松, 郁林海, 顾春飞, 等. 经脐入路腹腔镜胆总管探查一期缝合术后胆汁漏34例分析[J]. 肝胆胰外科杂志, 2014, 26(4):268–271.Feng LS, Yu LH, Gu CF, et al. Analysis of bile leakage after primary suture following transumbilical laparoscopic common bile duct exploration in 34 cases[J]. Journal of Hepatopancreatobiliary Surgery, 2014, 26(4):268–271.
[23] 孙长华, 白剑峰. 腹腔镜胆总管切开取石一期缝合术75例临床分析[J]. 腹腔镜外科杂志, 2014, 19(5):325–327.Sun CH, Bai JF. Clinical experience of laparoscopic choledocholithotomy and primary suture: a report of 75 cases[J].Journal of Laparoscopic Surgery, 2014, 19(5):325–327.
[24] 潘峥, 程张军, 刘胜利, 等. 胆总管结石腹腔镜胆总管探查术后一期缝合与T管引流的临床比较[J]. 中国普通外科杂志, 2015,24(8):1135–1139. doi:10.3978/j.issn.1005–6947.2015.08.016.Pan Z, Cheng ZJ, Liu SL, et al. Primary closure versus T-tube drainage following laparoscopic common bile duct exploration for choledocholithiasis[J]. Chinese Journal of General Surgery, 2015,24(8):1135–1139. doi:10.3978/j.issn.1005–6947.2015.08.016.
[25] Liu D, Cao F, Liu J, et al. Risk factors for bile leakage after primary closure following laparoscopic common bile duct exploration:a retrospective cohort study[J]. BMC Surg, 2017, 17(1):1. doi:10.1186/s12893–016–0201–y.
[26] Lu J, Xiong XZ, Cheng Y, et al. One-stage versus two-stage management for concomitant gallbladder stones and common bile duct stones in patients with obstructive jaundice[J]. Am Surg, 2013,79(11):1142–1148.