患者由于血中促聚集和促凝因子增加,而抗聚集、抗凝和纤溶机制受损,以及静脉瘀血、低蛋白血症、高脂血症、血液浓缩、血液黏滞度增加、激素和利尿剂的使用等原因引起血浆纤维蛋白原水平增高和纤维蛋白及纤维蛋白原降解产物含量显著上升等现象,最终使得蛋白C和蛋白S水平多正常或增高,但是其活性降低,从而产生了血液高凝状态[1]。大量报道[2-4]指出,与开腹手术相比,腹腔镜胆囊切除术的一些因素,诸如年龄偏大、伴高脂血症史、术前收缩压偏高、术前低密度脂蛋白胆固醇(low density lipoprotein cholesterol,LDL-C)水平偏高、CO2气腹、手术体位及入路方式均可影响术后血液高凝状态形成。然而,腹腔镜胆囊切除术也有自身劣势,诸如深静脉血栓形成、皮下气肿、更易诱发术后血液高凝状态等[5]。目前,缺乏重要的预测胆囊切除术后患者血液高凝状态形成的分子标记物,且关于影响腹腔镜胆囊切除术后患者血液高凝状态形成因素的相关研究较少。本研究将重点探讨影响腹腔镜胆囊切除术后患者血液高凝状态形成的标记物,为预防及治疗血液高凝状态提供证据。
1 资料与方法
1.1 研究对象
前瞻性选择2012年1月—2015年12月来我院接受腹腔镜胆囊切除术治疗的患者108例。根据患者术后24 h有无血液高凝状态发生分为高凝组(n=32)和非高凝组(n=76)。其中,高凝组男15例,女17例;年龄37~74岁,平均(59.35±12.51)岁,中位年龄62岁。非高凝组男31例,女45例;年龄38~70岁,平均(56.12±13.22)岁,中位年龄58岁。本研究获得我院医学伦理学委员会批准,且所有研究对象均知情同意。
1.2 纳入和排除标准
纳入标准:诊断符合中华医学会外科学分会胆道外科学组发布的《急性胆道系统感染的诊断和治疗指南(2011年版)》诊断标准[6];所有符合腹腔镜胆囊切除术适应证及禁忌证的患者;无其他脏器严重疾病患者;由患者知情同意并签署腹腔镜胆囊切除术知情同意书,提供患者的详细资料。排除标准:其它结石及并发症(急性胆囊炎、结石性胆囊炎、继发性胆总管结石)患者;伴有心、肝、脾、肺、肾、脑、造血系统等重要脏器损伤患者;有上腹部手术史患者;中、后期妊娠患者;难耐手术及凝血功能障碍患者;肿瘤及癌症患者;合并血液系统疾病或甲状腺功能亢进等其他疾病患者;精神、听力及语言障碍患者;随访资料丢失或不全患者;未签署腹腔镜胆囊切除术知情同意书患者。
1.3 研究方法
血液高凝状态诊断标准:纤维蛋白原(fibrinogen,Fbg)>2 g/L或凝血酶时间<17.8 s中其中1项;血小板计数(platelet count,PLT)>300×109/L、D-二聚体(D-dimer,D-D)>500 ng/L、凝血酶时间<11.8 s、活化部分凝血酶时间<30.8 s中其中2项[7]。
临床医生应根据病历信息及临床检查详细记录患者的年龄、性别、体质量指数(body mass index,BMI)、烟酒嗜好,高血压、高血脂、高血糖史和现状,测量术前舒张压及收缩压。抽取患者术前的清晨空腹静脉血2~10 mL,应用深圳雷杜公司RT7200全自动血液分析仪和日本奥林巴斯公司AU2700型全自动生化分析仪检测各生化指标,包括分子标志物Fbg、D-D、PLT、凝血酶原片段(F1+F2)、转铁蛋白(transferrin,Trf)、α-酸性糖蛋白(alpha acid glycoprotein,Orso)、C-反应蛋白(C-reactive protein,CRP)、白细胞介素6(interleukin 6,IL-6)、LDL-C、高密度脂蛋白胆固醇(high density lipoprotein cholesterol,HDL-C)水平。其中,IL-6、Orso、D-D、F1+F2、Trf采用双抗体夹心酶联免疫吸附法检测;CRP采用透射比浊法检测;Fbg采用免疫浊度法检测[8-9]。BMI计算公式:BMI=体质量(kg)/身高(m)2。吸烟史:一生中每天吸卷烟1支以上,连续或累计6个月。嗜酒史:连续饮酒6个月以上,每周饮酒量≥200 g。
1.4 统计学处理
所有数据均利用SPSS 19.0统计软件进行统计学分析。计量资料采用t检验,以均值±标准差( ±s)表示;计数资料采用秩和χ2检验或F检验,P<0.05为差异有统计学意义。单因素、多因素采用非条件Logistic回归进行分析,多分类变量以哑变量的形式进入回归模型,变量入选标准α≤0.05,剔除标准α>0.05。
±s)表示;计数资料采用秩和χ2检验或F检验,P<0.05为差异有统计学意义。单因素、多因素采用非条件Logistic回归进行分析,多分类变量以哑变量的形式进入回归模型,变量入选标准α≤0.05,剔除标准α>0.05。
2 结 果
2.1 两组患者临床特征比较
108例腹腔镜胆囊切除术患者中,32例(29.63%)发生血液高凝状态,76例(70.37%)未发生血液高凝状态。两组患者在有高血脂病史、术前收缩压、Fbg、D-D、PLT、F1 + F2、Trf、Orso、CRP、IL-6、LDL-C、HDL-C方面差异有统计学意义(均P<0.05),在性别、年龄、BMI、有吸烟史、有嗜酒史、有糖尿病史、有高血压病史、术前舒张压、手术时间、术中出血量方面差异无统计学意义(均P>0.05)。其中,高凝组在有高血脂病史比例、术前收缩压、Fbg、D-D、PLT、F1+F2、Trf、Orso、CRP、IL-6、LDL-C方面明显高于非高凝组,在HDL-C方面明显低于非高凝组(表1)。
表1 发生血液高凝状态与未发生血液高凝状态患者临床特征比较
Table 1 Comparison of the clinical features between patients with and without hypercoagulable state formation

注:1 mmHg=0.133 kPa
Note: 1 mmHg=0.133 kPa
因素 高凝组(n=32) 非高凝组(n=76) t/χ2 P性别[n(%)]男15(46.9) 31(40.8) 0.34 0.56女17(53.1) 45(59.2)年龄(岁,x±s) 59.35±12.51 56.12±13.22 -1.20 0.23 BMI(kg/m2,x±s) 26.15±2.14 26.38±2.24 0.50 0.62有吸烟史[n(%)] 9(28.1) 24(31.6) 0.13 0.72有嗜酒史[n(%)] 8(25.0) 22(28.9) 0.25 0.67有糖尿病史[n(%)] 6(18.8) 13(17.1) 0.28 0.62有高血压病史[n(%)] 8(25.0) 15(19.7) 0.37 0.54有高血脂病史[n(%)] 15(46.9) 19(25.0) 5.00 0.03术前收缩压(mmHg,x±s) 133.25±12.58 121.58±10.51 -4.61 <0.01术前舒张压(mmHg,x±s) 76.38±9.02 77.12±8.57 0.39 0.69 Fbg(g/L,x±s) 4.21±1.25 3.70±1.01 -2.04 0.04 D-D(µg/L,x±s) 112.58±30.57 91.54±27.15 -3.37 <0.01 PLT(×109/L,x±s) 246.95±24.11 210.68±21.57 -7.36 <0.01 F1+F2(nmol/L,x±s) 0.19±0.05 0.12±0.02 -7.65 <0.01 Trf(g/L,x±s) 2.34±1.02 1.90±1.04 -2.04 0.04 Orso(g/L,x±s) 0.92±0.15 0.77±0.17 -4.56 <0.01 CRP(mg/L,x±s) 1.91±0.22 1.15±0.18 -7.62 <0.01 IL-6(pg/mL,x±s) 1.86±0.27 1.38±0.31 -6.34 <0.01 LDL-C(mg/dL,x±s) 3.25±1.14 2.49±1.02 -8.55 <0.01 HDL-C(mg/dL,x±s) 1.01±0.26 1.52±0.40 7.87 <0.01手术时间(min,x±s) 105.26±25.95 109.64±30.52 0.15 0.84术中出血量(mL,x±s) 359.64±105.68 344.95±115.52 -0.28 0.74
2.2 影响腹腔镜胆囊切除术后患者血液高凝状态形成的单因素Logistic回归分析
单因素Logistic回归分析结果显示,年龄≥57.50岁、有高血脂病史、术前收缩压≥128.00 mmHg、Fbg≥3.95 g/L、D-D≥100.00 µg/L、PLT≥228.00×109/L、F1+F2≥0.16 nmol/L、Trf≥2.15 g/L、Orso≥0.85 g/L、CRP≥1.50 mg/L、IL-6≥1.50 pg/mL、LDL-C≥2.85 mg/dL、HDL-C≤1.25mg/dL与腹腔镜胆囊切除术后患者血液高凝状态形成有关(均P<0.05)(表2)。
表2 血液高凝状态形成因素的单变量Logistic回归分析
Table 2 Univariate Logistic analysis of the factors for hypercoagulable state formation
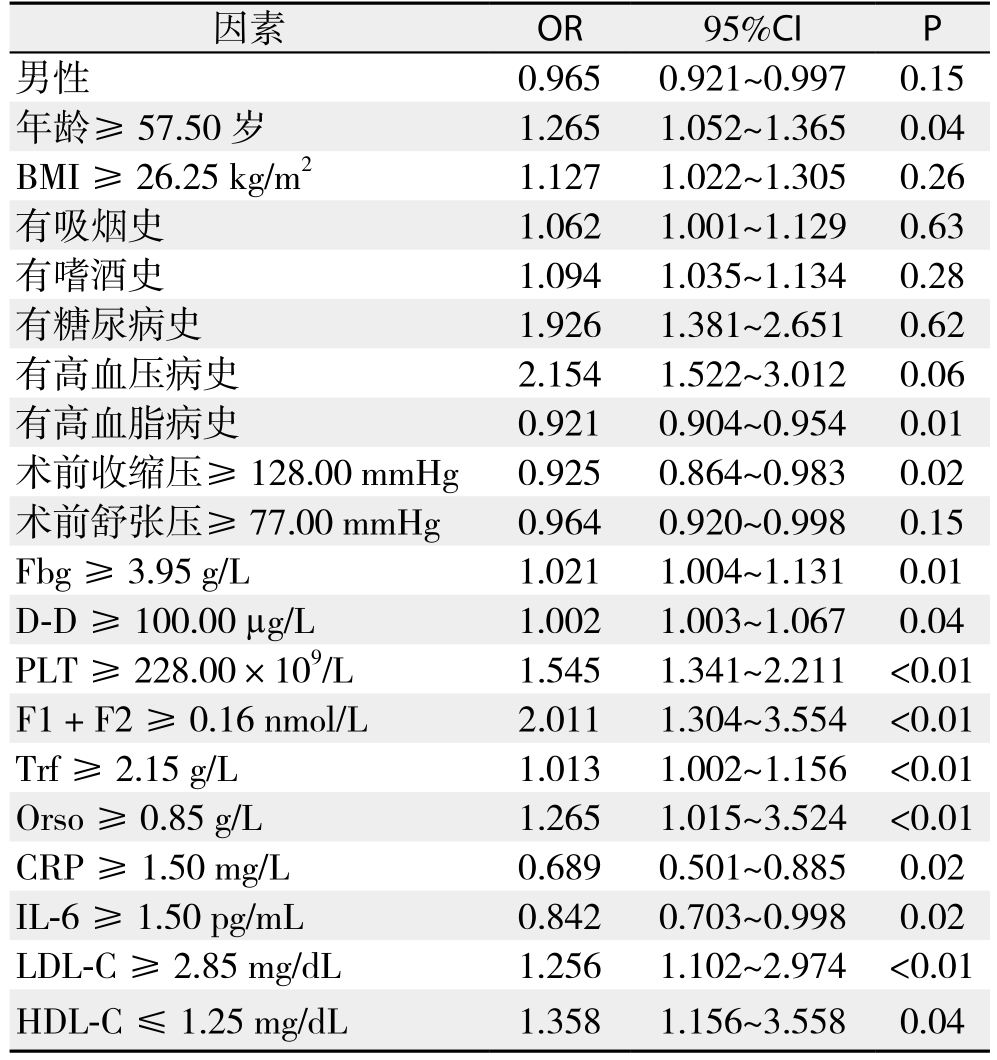
因素 OR 95%CI P男性 0.965 0.921~0.997 0.15年龄≥57.50岁 1.265 1.052~1.365 0.04 BMI≥ 26.25 kg/m2 1.127 1.022~1.305 0.26有吸烟史 1.062 1.001~1.129 0.63有嗜酒史 1.094 1.035~1.134 0.28有糖尿病史 1.926 1.381~2.651 0.62有高血压病史 2.154 1.522~3.012 0.06有高血脂病史 0.921 0.904~0.954 0.01术前收缩压≥128.00 mmHg 0.925 0.864~0.983 0.02术前舒张压≥77.00 mmHg 0.964 0.920~0.998 0.15 Fbg≥ 3.95 g/L 1.021 1.004~1.131 0.01 D-D ≥ 100.00 µg/L 1.002 1.003~1.067 0.04 PLT≥ 228.00×109/L 1.545 1.341~2.211 <0.01 F1 + F2≥ 0.16 nmol/L 2.011 1.304~3.554 <0.01 Trf≥ 2.15 g/L 1.013 1.002~1.156 <0.01 Orso≥ 0.85 g/L 1.265 1.015~3.524 <0.01 CRP≥1.50 mg/L 0.689 0.501~0.885 0.02 IL-6≥ 1.50 pg/mL 0.842 0.703~0.998 0.02 LDL-C ≥ 2.85 mg/dL 1.256 1.102~2.974 <0.01 HDL-C ≤ 1.25 mg/dL 1.358 1.156~3.558 0.04
2.3 影响腹腔镜胆囊切除术后患者血液高凝状态形成的多因素Logistic回归分析
多因素Logistic回归分析结果显示,有高血脂病史、Fbg≥3.95 g/L、D-D≥100.00 µg/L、PLT≥228.00×109/L、F1+F2≥0.16 nmol/L、Trf≥2.15 g/L、Orso≥0.85 g/L、CRP≥1.50 mg/L、IL-6≥1.50 pg/mL、LDL-C≥2.85 mg/dL是腹腔镜胆囊切除术后患者血液高凝状态形成的危险性因素(P<0.05)(表3)。
表3 血液高凝状态形成因素的多变量Logistic回归分析
Table 3 Multivariate Logistic analysis of the factors for hypercoagulable state formation
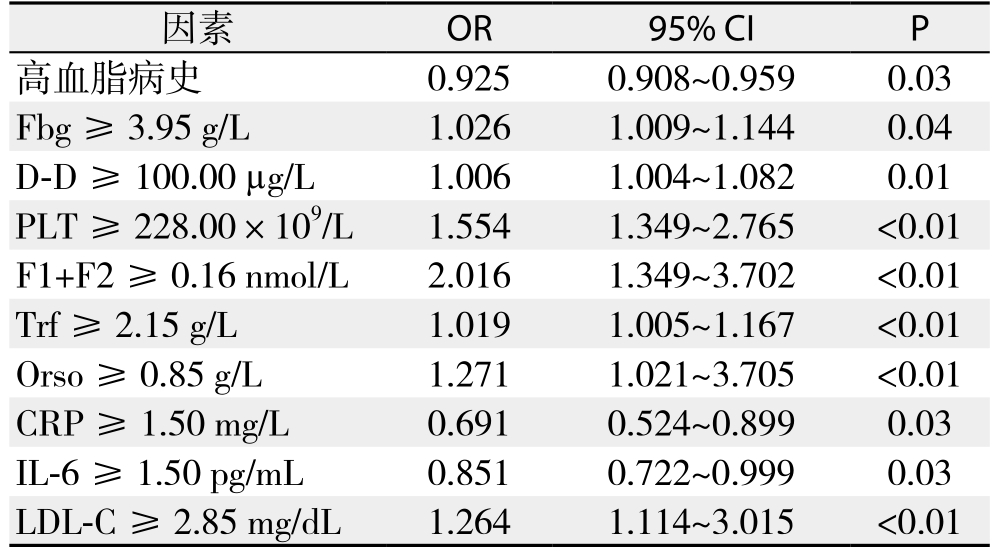
因素 OR 95% CI P高血脂病史 0.925 0.908~0.959 0.03 Fbg≥ 3.95 g/L 1.026 1.009~1.144 0.04 D-D ≥ 100.00 µg/L 1.006 1.004~1.082 0.01 PLT ≥ 228.00×109/L 1.554 1.349~2.765 <0.01 F1+F2≥ 0.16 nmol/L 2.016 1.349~3.702 <0.01 Trf≥ 2.15 g/L 1.019 1.005~1.167 <0.01 Orso≥ 0.85 g/L 1.271 1.021~3.705 <0.01 CRP≥1.50 mg/L 0.691 0.524~0.899 0.03 IL-6≥ 1.50 pg/mL 0.851 0.722~0.999 0.03 LDL-C≥2.85 mg/dL 1.264 1.114~3.015 <0.01
3 结 论
腹腔镜胆囊切除术是胆道外科常用的手术,分为由胆囊管开始的顺行切除和由胆囊底部开始的逆行切除两种[10]。传统的开腹胆囊切除术针对性差、伤口愈合慢、创伤大、易出现并发症,导致患者痛苦大、术后恢复不良等问题。腹腔镜胆囊切除手术凭借其切口小、创伤少、患者疼痛感轻、平均住院时间短等优势自开展以来,已迅速为外科医师及患者所接受。然而,腹腔镜胆囊切除术也有自身劣势,诸如深静脉血栓形成、皮下气肿、更易诱发术后血液高凝状态等。据报道[11],腹腔镜手术术后血液高凝状态的发生率约为35%,特别是对于合并有高血压、糖尿病及高脂血症等的高龄患者,进行腹腔镜手术对其术后血液高凝状态具有促进作用。目前,缺乏重要的预测胆囊切除术后患者血液高凝状态形成的分子标记物,且关于影响腹腔镜胆囊切除术后患者血液高凝状态形成因素的相关研究较少。本研究结果显示,有高血脂病史、Fbg≥3.95 g/L、D-D≥100.00 µg/L、PLT≥228.00×109/L、F1+F2≥0.16 nmol/L、Trf≥2.15 g/L、Orso≥0.85 g/L、CRP≥1.50 mg/L、IL-6≥1.50 pg/mL、LDL-C≥2.85 mg/dL是腹腔镜胆囊切除术后患者血液高凝状态形成的危险性因素。
张雁凯等[7]通过探讨腹腔镜胆囊切除术后患者血液高凝状态的危险因素,发现伴高脂血症、术前收缩压≥127 mmHg、术前LDL-C≥2.84 mmol/L的患者易发生血液高凝状态。梁節等[12]通过分析腹腔镜下胃癌手术后高凝血状态发生的监测及护理,发现腹腔镜下胃癌手术患者术后明显处于高凝血状态。钱永亮等[13]的研究也指出腹腔镜胃癌手术与开腹手术均会使患者血液处于高凝状态,但腹腔镜手术对患者凝血功能影响比开腹手术大。本研究中,有无高血脂病史,术前Fbg、D-D、PLT、F1+F2、Trf、Orso、CRP、IL-6、LDL-C水平是血液高凝状态形成的关键影响因素。有研究[14]指出,高脂血症可通过降低纤溶功能和提高凝血活性对患者机体产生影响,这或许是因为高脂血症患者的游离脂肪酸可提供激活的接触表面,增加大颗粒脂蛋白表面的电荷密度,并促使血浆凝血因子VII激活,从而加重血液凝固性。术前LDL-C水平作为血液高凝状态形成的影响因素是因为:氧化的LDL可影响机体一氧化氮的合成及凝血酶调节蛋白的活性,损害血管内皮功能;氧化的LDL还可形成泡沫细胞,与黏多糖结合形成不溶性沉淀,促使血栓及血液高凝状态形成[15-17]。D-D是纤维蛋白单体经活化因子XIII交联后,再经纤溶酶水解所产生的一种特异性降解产物,是一个特异性的纤溶过程标记物。脑梗死、心肌梗死、静脉血栓形成、肺栓塞、肿瘤、手术、弥漫性血管内凝血、感染及组织坏死等均可导致D-D升高[18-20]。急性胆道系统感染患者术前D-D、CRP、IL-6升高或许提示患者已发生感染及凝血。血栓前状态分子标志物F1+F2是在血液凝固的瀑布反应过程中,由因子Xa复合物水解凝血酶原后所生成的多肽片段[21-22]。Trf是血浆中主要的含铁蛋白质,负责运载由消化管吸收的铁和由红细胞降解释放的铁,供成熟红细胞生成[23]。Orso是主要的急性时相反应蛋白,在急性炎症时增高,与免疫防御功能密切相关[24-25]。上述术前分子标志物水平升高表明急性胆道系统感染患者病情已经进展,经腹腔镜胆囊切除术后利于患者血液高凝状态发生。
总之,有无高血脂病史,术前Fbg、D-D、PLT、F1+F2、Trf、Orso、CRP、IL-6、LDL-C水平与腹腔镜胆囊切除术后患者血液高凝状态形成关系密切。临床医师在诊治腹腔镜胆囊切除术患者过程中,应关注患者术前有无高血脂病史情况,对术前上述分子标志物水平偏高的患者更应格外注意,且对其他外科腹腔镜术后患者的影响还需要进一步深入研究。
参考文献
[1] Liu C, Guan Z, Xu Q, et al. Relation of thromboelastography parameters to conventional coagulation tests used to evaluate the hypercoagulable state of aged fracture patients[J].Medicine (Baltimore), 2016, 95(24):e3934. doi: 10.1097/MD.0000000000003934.
[2] Zezos P, Christoforidou A, Kouklakis G, et al. Coagulation and fibrinolysis activation after single-incision versus standard laparoscopic cholecystectomy: a single-center prospective casecontrolled pilot study[J]. Surg Innov, 2014, 21(1):22–31. doi:10.1177/1553350613484591.
[3] Ulrych J, Kvasnicka T, Fryba V, et al. 28 day post-operative persisted hypercoagulability after surgery for benign diseases: a prospective cohort study[J]. BMC Surg, 2016, 16:16. doi: 10.1186/s12893–016–0128–3.
[4] Enomoto T, Adachi S, Kurata M, et al. Two Cases of Cholecystectomy in the Hypercoagulable and Hyperfibrinoritic Condition after Aortic Endovascular Stent Graft Placement[J].Nihon Rinsho Geka Gakkai Zasshi, 2009, 63(6):1374–1378.
[5] Sharma A, Dahiya D, Kaman L, et al. Effect of various pneumoperitoneum pressures on femoral vein hemodynamics during laparoscopic cholecystectomy[J]. Updates Surg, 2016,68(2):163–169. doi: 10.1007/s13304–015–0344–x.
[6] 中华医学会外科学分会胆道外科学组. 急性胆道系统感染的诊断和治疗指南(2011版)[J]. 中华消化外科杂志, 2011, 10(1):9–13.doi:10.3760/cma.j.issn.1673–9752.2011.01.004.Biliary Surgery Group, Surgery Branch of Chinese Medical Association. Diagnosis and treatment guidelines for acute biliary infection (2011 edition)[J]. Chinese Journal of Digestive Surgery,2011, 10(1):9–13. doi:10.3760/cma.j.issn.1673–9752.2011.01.004.
[7] 张雁凯, 宫轲, 张成才, 等. 腹腔镜胆囊切除术后患者血液高凝状态的危险因素分析[J]. 中国医药, 2016, 11(2):250–254.doi:10.3760/cma.j.issn.1673–4777.2016.02.028.Zhang YK, Gong K, Zhang CC, et al. Analysis of risk factors of postoperative hypercoagulable status after laparoscopic cholecystectomy[J]. China Medicine, 2016, 11(2):250–254.doi:10.3760/cma.j.issn.1673–4777.2016.02.028.
[8] 何嗪, 黄国栋, 武艳, 等. 双歧杆菌四联活菌片联合头孢克肟对细菌性肠炎患者C反应蛋白、铜蓝蛋白、触珠蛋白及α1酸性糖蛋白的影响研究[J]. 中国生化药物杂志, 2015,(9):109–111.He Q, Huang GD, Wu Y, et al. Effect of Bifidobacterium tetravaccine tablets(live) combined with cefixime on C-reactive protein, ceruloplasmin, haptoglobin and α1-acid glycoprotein in patients with bacterial enteritis[J]. Chinese Journal of Biochemical Pharmaceutics, 2015,(9):109–111.
[9] 白敬恩, 李宏, 魏云彪. 左卡尼汀对维持血液透析患者炎症反应及营养状况的影响[J]. 中国临床实用医学, 2016, 7(4):32–34.doi:10.3760/cma.j.issn.1673–8799.2016.04.010.Bai JE, Li H, Wei YB, et al. Effect of L-carnitine on inlfammationand nutritional status of patients who underwent maintenance hemodialysis[J]. China Clinical Practical Medicine, 2016, 7(4):32–34. doi:10.3760/cma.j.issn.1673–8799.2016.04.010.
[10] Aytaç B, Cakar S. The outcome of gallbladder perforation during laparoscopic cholecystectomy[J]. Acta Chir Belg, 2003,103(4):388–391.
[11] 张成才. 腹腔镜手术对合并基础疾病患者凝血系统的影响[J]. 中国微创外科杂志, 2012, 12(4):372–375. doi:10.3969/j.issn. 1009–6604.2012.04.026.Zhang CC. Influence of laparoscopic surgery on coagulation system in patients with concomitant underlying disease[J]. Chinese Journal of Minimally Invasive Surgery, 2012, 12(4):372–375. doi:10.3969/j.issn.1009–6604.2012.04.026.
[12] 梁節. 腹腔镜下胃癌手术后血液高凝状态发生的监测及护理[J]. 血栓与止血学, 2017, 23(2):333–335. doi:10.3969/j.issn.1009–6213.2017.02.052.Liang J. Monitoring and nursing intervention of hypercoagulable state after laparoscopic gastric cancer surgery[J]. Chinese Journal of Thrombosis and Hemostasis, 2017, 23(2):333–335. doi:10.3969/j.issn.1009–6213.2017.02.052.
[13] 钱永亮. 腹腔镜胃癌手术与开腹手术对患者凝血功能影响的对比研究[J]. 中国现代药物应用, 2015, 9(9):52–53. doi:10.14164/j.cnki.cn11–5581/r.2015.09.032.Qian YL. Comparison of influence of laparoscopic and open gastric cancer surgery on coagulation system of the patients[J].Chinese Journal of Modern Drug Application, 2015, 9(9):52–53.doi:10.14164/j.cnki.cn11–5581/r.2015.09.032.
[14] Orlov SV, Domashenko MA, Kostyreva MV, et al. Hemorheology and hemostasis in patients suffering from ischemic cerebral stroke and metabolic syndrome[J]. Klin Med (Mosk), 2007, 85(1):40–44.
[15] 王刚林, 张淑香, 潘能科, 等. 小而密低密度脂蛋白胆固醇临床研究进展[J]. 检验医学与临床, 2015, 12(12):1804–1806.doi:10.3969/j.issn.1672–9455.2015.12.063.Wang GL, Zhang SX, Pan NK, et al. Clinical research progress on small dense low-density lipoprotein-cholesterol[J]. Laboratory Medicine and Clinic, 2015, 12(12):1804–1806. doi:10.3969/j.issn.1672–9455.2015.12.063.
[16] 庄华章, 陈永杰. 高凝状态相关指标在结直肠癌患者手术前后的变化及术式的影响[J]. 中国普通外科杂志, 2014, 23(4):458–461.doi:10.7659/j.issn.1005–6947.2014.04.011.Zhuang HZ, Chen YJ. Pre-and postoperative changes of parameters related to hypercoagulability in colorectal patients and the influence of mode of operation[J]. Chinese Journal of General Surgery, 2014,23(4):458–461. doi:10.7659/j.issn.1005–6947.2014.04.011.
[17] 徐亚玲, 常颖, 陈叙, 等. 妊娠期糖尿病孕妇妊娠晚期血脂及凝血功能指标检测结果分析[J]. 中国妇幼保健, 2017, 32(5):951–954.doi:10.7620/zgfybj.j.issn.1001–4411.2017.05.27.Xu YL, Chang Y, Chen X, et al. Analysis on the detection results of blood lipids and coagulation parameters in pregnant women with gestational diabetes mellitus during the third trimester of pregnancy[J]. Maternal & Child Health Care of China, 2017,32(5):951–954. doi:10.7620/zgfybj.j.issn.1001–4411.2017.05.27.
[18] Fukumoto K, Taniguchi T, Usami N, et al. Preoperative plasma D-D level is an independent prognostic factor in patients with completely resected non-small cell lung cancer[J]. Surg Today, 2015, 45(1):63–67. doi: 10.1007/s00595–014–0894–4.
[19] Nichenametla G, Thomas VS. Evaluation of Serum Pregnancy Associated Plasma Protein-A & Plasma D-D in Acute Coronary Syndrome[J]. J Clin Diagn Res, 2016, 10(1):BC01–3. doi: 10.7860/JCDR/2016/14432.7011.
[20] Ali NMA, Gameel FEMH, Elsayid M, et al. Alterations in D-D,Prothrombin Time and Activated Partial Thromboplastin Time as Thrombogenesis Activity Markers in Patients with Acute Myocardial Infarction[J]. OJBD, 2016, 6(1):1–5.
[21] Hagii J, Tomita H, Metoki N, et al. Effect of rivaroxaban on prothrombin fragment 1+2 compared with warfarin in patients with acute cardioembolic stroke: Insight from its serial measurement[J].Thromb Res, 2016, 148:9–14. doi: 10.1016/j.thromres.2016.10.011.
[22] Kubo T, Takashi T, Ashikari M, et al. Two Tightly Linked Genes at the hsa1 Locus Cause Both F1 and F2 Hybrid Sterility in Rice[J].Mol Plant, 2016, 9(2):221–232. doi: 10.1016/j.molp.2015.09.014.
[23] de Swart L, Hendriks JC, van der Vorm LN, et al. Second international round robin for the quantification of serum nontransferrin-bound iron and labile plasma iron in patients with ironoverload disorders[J]. Haematologica, 2016, 101(1):38–45. doi:10.3324/haematol.2015.133983.
[24] Ayyub A, Saleem M, Fatima I, et al. Glycosylated Alpha-1-acid glycoprotein 1 as a potential lung cancer serum biomarker[J] Int J Biochem Cell Biol, 2016, 70:68–75. doi: 10.1016/j.biocel.2015.11. 006.
[25] Ajmal MR, Abdelhameed AS, Alam P, et al. Interaction of new kinase inhibitors cabozantinib and tofacitinib with human serum alpha-1 acid glycoprotein. A comprehensive spectroscopic and molecular Docking approach[J]. Spectrochim Acta A Mol Biomol Spectrosc, 2016, 159:199–208. doi: 10.1016/j.saa.2016.01.049.