20余年来,随着腹腔镜胃癌根治术技术的不断成熟进步,其用于治疗进展期胃癌取得的良好近期疗效及术后早期微创优势明显[1-5],多项回顾性研究报道其远期疗效不劣于传统开腹手术[6-8]。由于胃周的解剖层面多,血供丰富,胃周淋巴结清扫难度大,腹腔镜手术操作又有其自身的特殊性,而腹腔镜胃癌根治术的手术入路各有特点。目前,有Hyung等[9-10]采用右侧站位右侧入路和李国新等[11-13]采用左侧站位中间入路等手术入路方式,但这几种入路方式在胰腺上区淋巴结清扫相似,清扫难度大,受到胃后壁阻挡,视野显露困难。本文结合笔者所在中心既往腹腔镜胃癌根治术胃周淋巴结清扫的经验和相关文献资料,回顾性分析2016年1月—2017年7月广东省中医院胃肠外科36例患者实施完全左侧入路腹腔镜根治性全胃切除术,报告并探讨其安全性和可行性。
1 资料与方法
1.1 一般资料
收集2016年1月—2017年7月实施完全左侧入路腹腔镜根治性全胃切除术36例临床资料,其中男20例,女16例;平均年龄为(61.7±13.3)岁;体质量指数平均为(21.8±4.2)kg/m2;胃上部癌19例,胃中部癌17例。所有患者术前均经胃镜病理诊断为胃腺癌,术前胸腹部CT检查未见远处转移。术前肿瘤分期:IIA期4例(11.1%),IIB期7例(19.4%),IIIA期10例(27.8%),IIIB期9例(25.0%),IIIC期6例(16.7%)。术前所有患者经美国麻醉医师协会(ASA)评分为I~III。本研究中手术方法经伦理委员会审批通过,术前由患者或被授权家属签署知情同意书。
1.2 手术方法
1.2.1 探查 采用“弧形五孔法”[14],气腹压力维持在 12~14 mmHg(1 mmHg=0.133 kPa),置入肝拉钩挡肝(图1A)。探查腹腔,排查腹膜、网膜和其余脏器表面有无转移病灶,原发肿瘤位于胃中上部。
1.2.2 手术步骤 ⑴ 左侧入路:术者站于患者两腿之间,助手位于患者右侧,持镜手位于一助右侧。患者于头高脚低右侧倾斜15~20°,充分暴露左上腹手术区域。助手将左侧大网膜向头侧掀起,术者沿横结肠上缘于其中部偏左进入,充分切开胃结肠韧带(图1B),进入网膜囊(若行联合网膜囊切除则循囊外间隙分离左侧横结肠系膜前叶及胰尾胰腺被膜),向左分离大网膜至结肠脾曲,达脾下极,并优先离断“罪恶韧带”[15],将胃大弯向右牵引,显露脾门与胃大弯间隙,游离至胰尾上缘,显露脾动静脉,于胰尾处显露胃网膜左血管并于根部离断,清扫第4sb组淋巴结(图1C)。按“黄氏三步法”[16-17]清扫脾门淋巴结方法清扫第10组淋巴结(图1D),并根部离断胃短血管,清扫第4sa组淋巴结,紧贴脾动脉干裸化胃后血管并离断,清扫第11组淋巴结(图1E)。向右下方牵拉胃底体部胃壁,显露贲门左侧区域,沿左侧膈肌角分离膈胃韧带,并进一步裸化食管下段左侧,彻底完成第2组淋巴结清扫(图1F)。将胃体翻至右侧,并继续沿脾动脉显露肝总动脉及腹腔动脉干,自左向右清扫7、8a、9组淋巴结(图1G),顺势清扫第5、12a组淋巴结。主刀移至患者左侧,持镜手站于患者两腿之间,掀起胃体,继续自左向右分离右侧大网膜(图1H)。⑵ 右侧分离:于胰头前显露胃结肠共同干,断扎胃网膜右静脉,继续向十二指肠内侧游离,于根部断扎胃网膜右动脉,清扫第6组淋巴结。沿胰头表面向上清扫,裸化十二指肠下缘及后方。⑶ 小弯侧清扫:翻转胃体,贴近肝脏下缘切开肝胃韧带,剪开肝十二指肠韧带浆膜,于根部断扎胃右动静脉,彻底完成第5,12a组淋巴结清扫(图1I-J)。继续向左分离切断肝胃韧带及分离贲门右脂肪淋巴组织,彻底清扫第1、3组淋巴结(图1K)。⑷ 消化道重建:经完全左侧入路完成胃周游离、淋巴清扫,将胃连十二指肠球部、大小网膜、及周围脂肪淋巴组织完整切除,取出标本(图1L),在腹腔镜下行食管空肠Roux-en-Y吻合术,完成消化道重建。
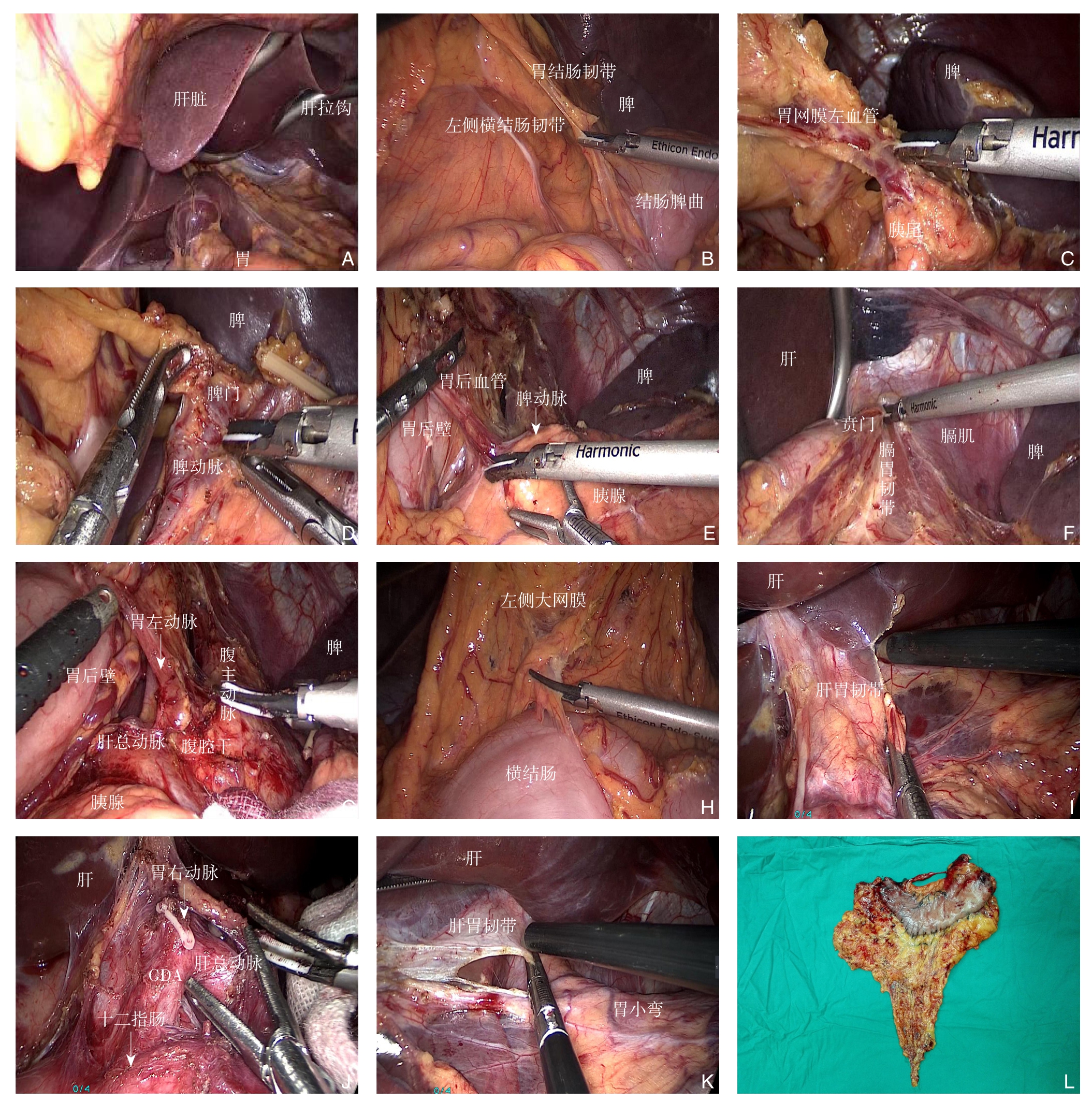
图1 术中处理 A:置入肝拉钩挡肝;B:左侧入路,切开胃结肠韧带;C:显露胰腺上缘,清扫第4sb组淋巴结;D:沿脾血管清扫第10组淋巴结;E:沿脾动脉裸化胃后壁,清扫第11组淋巴结;F:分离膈胃韧带,清扫第2组淋巴结;G:胃体翻至右侧,自左向右,清扫第7、8a、9组淋巴结;H:自左向右,分离右侧大网膜;I:沿肝脏下缘切开肝胃韧带;J:彻底清扫第5、12a组淋巴结;K:向左分离肝胃韧带及贲门右脂肪淋巴组织,清扫第1、3组淋巴结;L:全胃标本
Figure 1 Intraoperative views A: Placement of liver retractor for keeping out the liver; B: Entering via left approach and incision of the gastrocolic ligament; C: Exposure of the superior border of the pancreas and clearance of the station no.4sb lymph nodes; D: Clearance of the station no.10 lymph nodes along the splenic vessels; E: Denuding the posterior wall of the stomach along the splenic artery and clearance of the station no.11 lymph nodes; F: Separation of the gastrophrenic ligament and clearance of the station no.2 lymph nodes;G: Turning the body of the stomach to the right side, and clearance of the station no.7, 8a and 9 lymph nodes from left to right; H:Division of the right great omentum with a left to right direaction; I: Incision of the hepatogastric ligament along the interior border of the liver; J: Thorough clearance of the station no.5 and 12a lymph nodes; K: Dissection of the fat and lymph tissues around the hepatogastric ligament and gastric cardia, and clearance of the station no.1 and 3 lymph nodes; L: Specimen of the whole stomach
1.3 数据处理
本研究仅涉及统计描述,计数资料用均数±标准差( )表示,计量资料用率表示。
)表示,计量资料用率表示。
2 结 果
2.1 手术情况
全组36例患者均手术成功,无中转开腹,术中无联合脾脏等脏器切除及相关并发症,术后无严重手术相关并发症。手术时间为(228.6±45.9)min,术中出血量(82.7±25.5)mL。
2.2 术后恢复情况
肛门自主排气时间(47.2±15.7)h,术后进食全流时间(72.6±20.1)h,首次下床活动时间(36.5±4.5)h,术后住院时间(9.5±1.5)d。
2.3 术后病理
手术近端切缘为(4.2±1.8)cm,所有标本切缘均为阴性,淋巴结清扫数目(35.5±6.2)枚,其中淋巴结阳性数目为(3.9±2.1)枚,肿瘤分期:IIA期4例(8.3%),IIB期7例(16.7%),IIIA期10例(33.3),IIIB期9例(25.0%),IIIC期6例(16.7%)。
2.4 术后并发症
术后2例(5.6%)切口感染,2例(5.6%)炎性肠梗阻,1例(2.8%)发生肺部感染,均经对症保守治疗后痊愈出院。
3 讨 论
腹腔镜胃癌根治术在日本、韩国及中国已得到广泛开展,成为早期胃癌的常用术式之一[18-20]。随着腹腔镜胃癌根治术的技术不断成熟,腹腔镜胃癌根治术也逐渐应用于进展期胃癌,其在远端胃癌根治术中的安全性获得认可[21-23],而目前对全胃根治术报道不多。由于胃周解剖层次多、胃癌淋巴结转移途径复杂及腹腔镜手术本身存在牵拉暴露不足等缺陷,对于进展期胃癌,要实现腹腔镜胃癌根治术非常困难。
目前,对于腹腔镜胃癌根治术,右侧站位右侧入路术者的位置、手术次序与开腹手术相仿,符合术者习惯,且先离断十二指肠使清扫第5、12组淋巴结时术野更开阔[24],但在清扫第7、8a、9组淋巴结时需要助手全程将胃托起暴露胃后壁,显露胃后血管、脾血管、及肝门区血管困难,增加清扫难度,且脾门血管后方显露困难,造成脾门血管后方淋巴结清扫困难。助手站于患者左侧,其右手大部分时间往往只起牵拉暴露作用,需左手配合主刀进行精细操作,对助手要求高,没有配合熟练的助手,很难完成右侧入路淋巴结清扫。
左侧站位中间入路在清扫第7、8a、9组淋巴结时,与右侧站位右侧入路相似,需要全程在胃后壁将胃托起,受胃后壁阻挡,视野显露困难,且对助手要求较高,如助手显露不好,将给此区域淋巴结清扫带来极大困难。
本中心采用完全左侧入路腹腔镜根治性全胃切除术,主刀站于患者两腿之间,不离断脾胃韧带,而优先分离“罪恶韧带”,有利于助手牵拉暴露脾门,可更容易彻底的清扫脾门淋巴结,并可使脾门淋巴结与切除的肿瘤标本一并切除,符合整块切除原则。在清扫完第4sa、10、11、2组淋巴结后,将胃体翻至右侧,可良好的显露肝总动脉、腹腔动脉干及胃左动脉,避免胃体及大网膜干扰,操作空间较大,更有利于清扫此区域第7、8a、9组淋巴结。同时结合本研究结果,采用完全左侧入路腹腔镜根治性全胃切除术,操作平面连贯,可减少更换操作平面次数,在胰腺上区清扫优势明显,显露难度小,可以充分暴露胰腺上缘,清扫安全,研究中36例患者,行胰腺上区清扫均未出现周围脏器损伤及出血等并发症。
右侧站位右侧入路、左侧站位中间入路托起胃体,暴露胰腺上区时,对肿瘤形成挤压压力大,特别是位于胃后壁肿瘤,容易直接接触,而本中心采用完全左侧入路,只需要牵拉网膜将胃体翻至右侧就可良好显露胰腺上区,可减少挤压触碰肿瘤的可能。
日本《胃癌处理规约规定》,对于进展期胃中上部癌,脾门淋巴结清扫属于D2淋巴结清扫的范围[25]。本研究在筛查入组标准时均选用进展期胃中上部癌,均接受脾门淋巴结清扫。在清扫脾门淋巴结时,本入路方式对于脾门后方淋巴结清扫仍存在一定局限性。
对于全胃切除术D2淋巴结整体清扫,安全有效的实施完全左侧入路腹腔镜根治性全胃切除术还需要注意以下几点:⑴ 建立一支长期稳定、配合默契的腹腔镜手术团队能有效地缩短手术时间,提高手术质量;⑵ 熟识胃周血管、脾门区血管解剖及邻近组织结构;⑶ 术前完善相关检查,多学科讨论会诊,充分评估手术相关风险,可通过CT三维血管重建充分了解脾门血管走形,可大大降低手术风险及手术时间[26];⑷ 团队成员要善于在实践中总结经验教训,改正不足,并根据手术录像,进行经常性、多向性经验交流,形成程序化的手术步骤。
综上所述,完全左侧入路腹腔镜根治性全胃切除术是安全的、可行的,符合肿瘤学根治原则。且应用完全左侧入路腹腔镜根治性全胃切除术,显露良好,操作简单,有助于缩短学习曲线,然而其远期疗效还有待进一步研究。
[1]Orsenigo E, Di Palo S, Tamburini A, et al.Laparoscopy-assisted gastrectomy versus open gastrectomy for gastric cancer: a monoinstitutional Western center experience[J].Surg Endosc, 2011,25(1):140–145.doi: 10.1007/s00464–010–1147–2.
[2]Koeda K, Nishizuka S, Wakabayashi G.Minimally invasive surgery for gastric cancer: the future standard of care[J].World J Surg,2011, 35(7):1469–1477.doi: 10.1007/s00268–011–1051–5.
[3]李恩, 吴祖光, 李志旺, 等.腹腔镜与开腹保脾脾门淋巴结清扫在进展期胃中上部癌中的疗效评价[J].新医学, 2016, 47(7):485–489.doi:10.3969/j.issn.0253–9802.2016.07.014.Li E, Wu ZG, Li ZW, et al.Evaluation of clinical efficacy of laparoscopic and open spleen-preserving splenic hilar lymph node dis-section for advanced middle-proximal gastric cancer[J].New Medicine, 2016, 47(7):485–489.doi:10.3969/j.issn.0253–9802.2016.07.014.
[4]陈钶, 牟一平, 徐晓武, 等.完全腹腔镜与开腹根治性全胃切除术的临床对照研究[J].中华外科杂志, 2013, 51(1):22–25.doi:10.3760/cma.j.issn.0529–5815.2013.01.007.Chen K, Mou YP, Xu XW, et al.The clinical comparison of totally laparoscopic versus open total gastrectomy for gastric cancer[J].Chinese Journal of Surgery, 2013, 51(1):22–25.doi:10.3760/cma.j.issn.0529–5815.2013.01.007.
[5]柳国富, 柯志刚, 徐江浩, 等.完全腹腔镜与开腹全胃切除的疗效及术后并发症分析[J].中国普通外科杂志, 2017, 26(10):1324–1329.doi:10.3978/j.issn.1005–6947.2017.10.016.Liu GF, Ke ZG, Xu JH, et al.Totally laparoscopic versus open radical gastrectomy: an analysis of efficacy and postoperative complications[J].Chinese Journal of General Surgery, 2017,26(10):1324–1329.doi:10.3978/j.issn.1005–6947.2017.10.016.
[6]Ohtani H, Tamamori Y, Noguchi K, et al.A meta-analysis of randomized controlled trials that compared laparoscopy-assisted and open distal gastrectomy for early gastric cancer.[J].J Gastrointest Surg.2010 Jun;14(6):958–964.doi: 10.1007/s11605–010–1195-x.
[7]Hamabe A, Omori T, Tanaka K, et al.Comparison of long-term results between laparoscopy-assisted gastrectomy and open gastrectomy with D2 lymph node dissection for advanced gastric cancer[J].Surg Endosc, 2012, 26(6):1702–1709.doi: 10.1007/s00464–011–2096–0.
[8]Kim HH, Han SU, Kim MC, et al.Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study[J].J Clin Oncol, 2014,32(7):627–633.doi: 10.1200/JCO.2013.48.8551.
[9]Hyung WJ, Lim JS, Song J, et al.Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer[J].J Am Coll Surg, 2008, 207(2):e6–11.doi: 10.1016/j.jamcollsurg.2008.04.027.
[10]Kim HH, Hyung WJ, Cho GS, et al.Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective,randomized Trial (KLASS Trial)[J].Ann Surg, 2010, 251(3):417–420.doi: 10.1097/SLA.0b013e3181cc8f6b.
[11]李国新.腹腔镜辅助远端胃癌D2根治术[J].消化肿瘤杂志:电子版, 2010, 2(4):249–254.Li GX.Laparoscopic radical resection (D2) of distal gastric cancer[J].Journal of Digestive Oncology: Electronic Version, 2010,2(4):249–254.
[12]李国新, 张策, 余江.腹腔镜辅助远端胃癌D2根治术:基于解剖的艺术[J].外科理论与实践, 2007, 12(6):533–538.doi:10.3969/j.issn.1007–9610.2007.06.007.Li GX, Zhang C, Yu J.Laparoscopic assisted D2 distal gastrectomy[J].Journal of Surgery Concepts & Practice, 2007,12(6):533–538.doi:10.3969/j.issn.1007–9610.2007.06.007.
[13]王道荣, 鱼海峰, 赵建国, 等.中间入路腹腔镜下进展期胃癌D2术62例分析[J].中华普外科手术学杂志: 电子版, 2010, 4(2):149–154.doi:10.3969/cma.j.issn.1674–3946.2010.02.009.Wang DR, Yu HF, Zhao JG, et al.Laparoscopic-assisted radical gastrectomy with a medial-to-lateral approach for advanced gastric carcinoma and D2 lymphadenectomy[J].Chinese Journal of Operative Procedures of General Surgery: Electronic Version, 2010,4(2):149–154.doi:10.3969/cma.j.issn.1674–3946.2010.02.009.
[14]钱锋, 唐波, 余佩武,等.腹腔镜胃癌手术的路径[J].中华消化外科杂志, 2010, 9(4):299–302.doi:10.3760/cma.j.issn.1673–9752.2010.04.021.Qian F, Tang B, Yu PW, et al.Operation path of laparoscopyassisted gastrectomy[J].Chinese Journal of Digestive Surgery, 2010,9(4):299–302.doi:10.3760/cma.j.issn.1673–9752.2010.04.021.
[15]王伟, 熊文俊, 李金, 等."罪恶韧带"在腹腔镜胃癌手术中预防脾损伤的临床价值[J].中华胃肠外科杂志, 2017, 20(8):887–890.doi:10.3760/cma.j.issn.1671–0274.2017.08.013.Wang W, Xiong WJ, Li J, et al.Criminal fold priority separating reduces splenic injury in laparoscopic radical gastrectomy[J].Chinese Journal of Gastrointestinal Surgery, 2017, 20(8):887–890.doi:10.3760/cma.j.issn.1671–0274.2017.08.013.
[16]陈起跃, 黄泽宁, 黄昌明,等.“黄氏三步法”在进展期胃上部癌腹腔镜保脾脾门淋巴结清扫术中的应用[J].中华消化外科杂志, 2015, 14(3):187–191.doi:10.3760/cma.j.issn.1673–9752.2015.03.004.Chen QY, Huang ZN, Huang CM, et al.Application of Huang's three-step maneuver for laparoscopic spleen-preserving splenic hilus lymphadenectomy for advanced proximal gastric cancer[J].Chinese Journal of Digestive Surgery, 2015, 14(3):187–191.doi:10.3760/cma.j.issn.1673–9752.2015.03.004.
[17]黄昌明, 林建贤.全腹腔镜胃癌根治术规范化实施策略与技术难点[J].中国实用外科杂志, 2016, 36(9):925–928.Huang CM, Lin JX.Standardization and technical tips in totally laparoscopic gastrectomy for gastric cancer[J].Chinese Journal of Practical Surgery, 2016, 36(9):925–928.
[18]陈敬洪, 陈家阳, 林汉昇, 等.28例腹腔镜胃癌根治术临床应用分析[J].中国社区医师: 医学专业, 2011, 13(32):63.doi:10.3969/j.issn.1007–614x.2011.32.057.Chen JH, Chen JY, Lin HS, et al.Clinical analysis of laparoscopic radical gastrectomy in 28 cases[J].Chinese Community Doctors,2011, 13(32):63.doi:10.3969/j.issn.1007–614x.2011.32.057.
[19]余佩武, 罗华星.腹腔镜胃癌手术规范化治疗[J].中华普外科手术学杂志:电子版, 2013, 7(1):10–12.doi:10.3877/cma.j.issn.1674–3946.2013.01.003.Yu PW, Luo HX.Standardized procedures of laparoscopic gastrectomy for gastric cancer[J].Chinese Journal of Operative Procedures of General Surgery: Electronic Version, 2013, 7(1):10–12.doi:10.3877/cma.j.issn.1674–3946.2013.01.003.
[20]中华医学会外科学分会腹腔镜与内镜外科学组.腹腔镜胃癌根治术手术入路选择专家共识[J].中国实用外科杂志, 2017,37(4):412–414.Group of Laparoscopic and Endoscopic Surgery, Society of Surgery,Chinese Medical Association.Expert consensus on selection of approaches for laparoscopic radical gastrectomy[J].Chinese Journal of Practical Surgery, 2017, 37(4):412–414.
[21]Dulucq JL, Wintringer P, Stabilini C, et al.Laparoscopic and open gastric resections for malignant lesions: a prospective comparative study[J].Surg Endosc, 2005, 19(7):933–938.doi: 10.1007/s00464–004–2172–9.
[22]Shinohara T, Satoh S, Kanaya S, et al.Laparoscopic versus open D2 gastrectomy for advanced gastric cancer: a retrospective cohort study[J].Surg Endosc, 2013, 27(1):286–294.doi: 10.1007/s00464–012–2442-x.
[23]张兵, 虞黎明, 赖斌, 等.远端胃癌完全腹腔镜手术对比腹腔镜辅助手术的Meta分析[J].中国普通外科杂志, 2014, 23(4):405–411.doi:10.7659/j.issn.1005–6947.2014.04.001.Zhang B, Yu LM, Lai B, et al.Totally laparoscopic versus laparoscopically assisted surgery for distal gastric cancer: a Metaanalysis[J].Chinese Journal of General Surgery, 2014, 23(4):405–411.doi:10.7659/j.issn.1005–6947.2014.04.001.
[24]Han HS, Kim YW, Yi NJ, et al.Laparoscopy-assisted D2 subtotal gastrectomy in early gastric cancer[J].Surg Laparosc Endosc Percutan Tech, 2003, 13(6):361–365.
[25]Japanese Gastric Cancer Association.Japanese classification of gastric carcinoma: 3rd English edition[J].Gastric Cancer, 2011,14(2):101–112.doi: 10.1007/s10120–011–0041–5.
[26]Wang JB, Huang CM, Zheng CH, et al.Role of 3DCT in laparoscopic total gastrectomy with spleen-preserving splenic lymph node dissection[J].World J Gastroenterol, 2014, 20(16):4797–4805.doi: 10.3748/wjg.v20.i16.4797.
