近期的临床统计资料显示,胆囊结石患者常合并胆总管结石,其发生率约为10%~18%[1],其发病率随年龄增长逐渐升高,61~70岁的患者达到31%,71~80岁的患者达到48%[2]。对于这类患者的治疗,目前很多学者采用腹腔镜胆囊切除(laparoscopic cholecystectomym,LC)联合术中经内镜逆行性胰胆管造影术(intraoperative endoscopic retrograde cholangiopancreatography,IOERCP)的方式,该方法与其他方法一样安全有效,且具有恢复快、住院时间短等优点[3-7]。笔者设计了一项前瞻性研究(通过医院伦理委员会审批,审批号:2015年审010-1号),与LC联合腹腔镜胆总管探查取石(laparoscopic common bile duct exploration,LCBDE)对比分析LC+IOERCP治疗老年胆囊结石合并胆总管结石安全性及疗效。
1 资料与方法
1.1 临床资料
将我院2015年5月—2017年10月收治的老年胆囊结石合并胆总管结石患者根据纳入和排除标准,共选择82例。按照随机数字表的方法随机分为两组,其中LC+IOERCP组42例,LC+LCBDE组40例。
纳入标准:⑴ 有上腹痛病史,伴或不伴发热、黄疸;⑵ 年龄在60岁以上;⑶ 术前肝功能异常,经B超、CT或核磁共振胰胆管成像(MRCP)等影响学检查明确为胆囊结石合并胆总管结石;⑷ 影像学检查可疑,LC时术中胆道造影证实胆总管结石。排除标准:⑴ 胆总管最大结石直径>15 mm;⑵ 严重心肺疾病无法耐受手术,有手术禁忌证者;⑶ 既往上腹手术史,可能腹腔内有严重粘连,而不宜行腹腔镜手术者;⑷ Mirrizi综合征,合并肝内型肝胆管结石、胆道肿瘤或其他肿瘤者;⑸ 伴有幽门梗阻或行毕II氏胃大部切除术,而行ERCP困难者;⑹ 对造影剂过敏者;⑺ 伴有重症急性胆源性胰腺炎患者。
1.2 手术方法
LC+IOERCP组:采用腹腔镜内镜会师技术(laparoendoscopic rendezvous,LERV):患者口服胃镜胶浆后,常规气管插管全身麻醉,口腔预留内镜牙垫。患者取仰卧位,采用三孔法行LC,术中维持气腹压在10~12 mmHg(1 mmHg=0.133 kPa),电勾解剖胆囊三角区,游离出胆囊动脉及胆囊管,可吸收夹钳夹胆囊动脉并将其切断,于胆囊管的远端上钛夹1枚,暂不切断胆囊管,电勾剥离胆囊,胆囊床用电凝止血。剪刀剪开部分胆管侧胆囊管,由右侧季肋部戳孔处置入弓形乳头切开刀,经胆囊管开口插入胆总管,行胆道造影确认插管成功后,经弓形刀插入斑马导丝,X线监视下将斑马导丝送至十二指肠肠腔。ERCP术者开始进行内镜操作,将患者头偏向左侧,保持仰卧位不变,将十二指肠镜经口、食道、胃送入十二指肠降段,拉直镜身,寻找到乳头及导丝,用取石网篮套住导丝,经十二指肠镜活检孔道拉出。顺导丝将弓形切开刀插入胆总管,将导丝自切开刀内拉出,在X线监视下将头端顺切开刀插入肝内胆管。腹腔镜组术者拔除弓形刀,可吸收夹夹闭胆囊管近端,切断胆囊管,取出胆囊,常规安置腹腔引流管,缝合切口。ERCP组术者根据胆管结石大小适当切开乳头或做气囊扩张,在X线监视下用取石网蓝及取石气囊取出结石,常规安置鼻胆管引流(图1)。
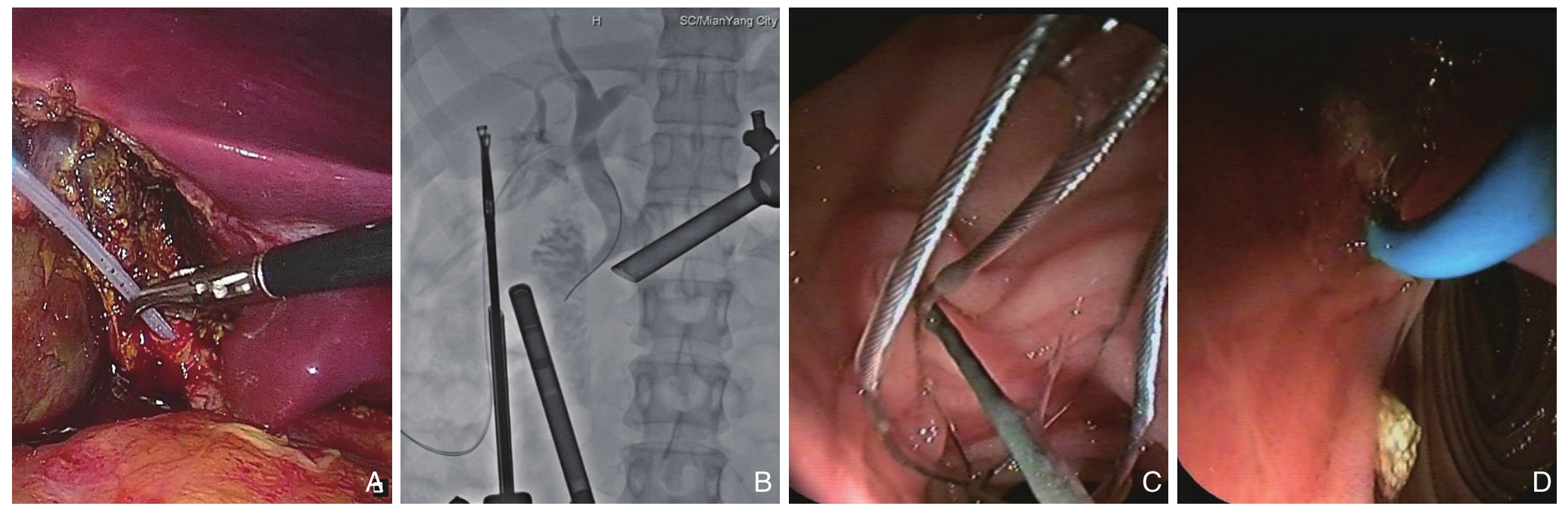
图1 LC+IOERCP组术中图片 A:将切开刀及导丝经胆囊管插入胆总管;B:术中胆道造影并将导丝通过乳头;C:将通过乳头的导丝拉出;D:取出胆总管内结石
Figure 1 Intraoperative view of the LC+IOERCP group A: Insertion of the papillotome and the guide wire into the common bile duct via the cystic duct; B: Intraoperative cholangiography and steering the guide wire through the papilla; C: Pulling the guide wire out of the papilla; D: Extraction of the stones in the common bile duct
LC+LCBDE组:常规气管插管全身麻醉,患者取仰卧位,消毒铺巾后,采用四孔法操作,分离胆囊周围粘连,解剖胆囊三角区,游离出胆囊管及胆囊动脉,分别钳夹后切断,电勾剥离胆囊,胆囊床电凝止血。显露出胆总管前壁,于胆囊管汇合水平用电勾纵行切口胆总管前壁1~2 cm,将胆道镜自剑突下Trocar置入,探查胆管并取出胆管内结石。根据胆管直径粗细,放置18~22 F的T管,4-0可吸收线间断缝合胆管壁切口,并自T管长臂冲水检查胆管缝合口无漏水后,安置腹腔引流管于温氏孔(图2)。
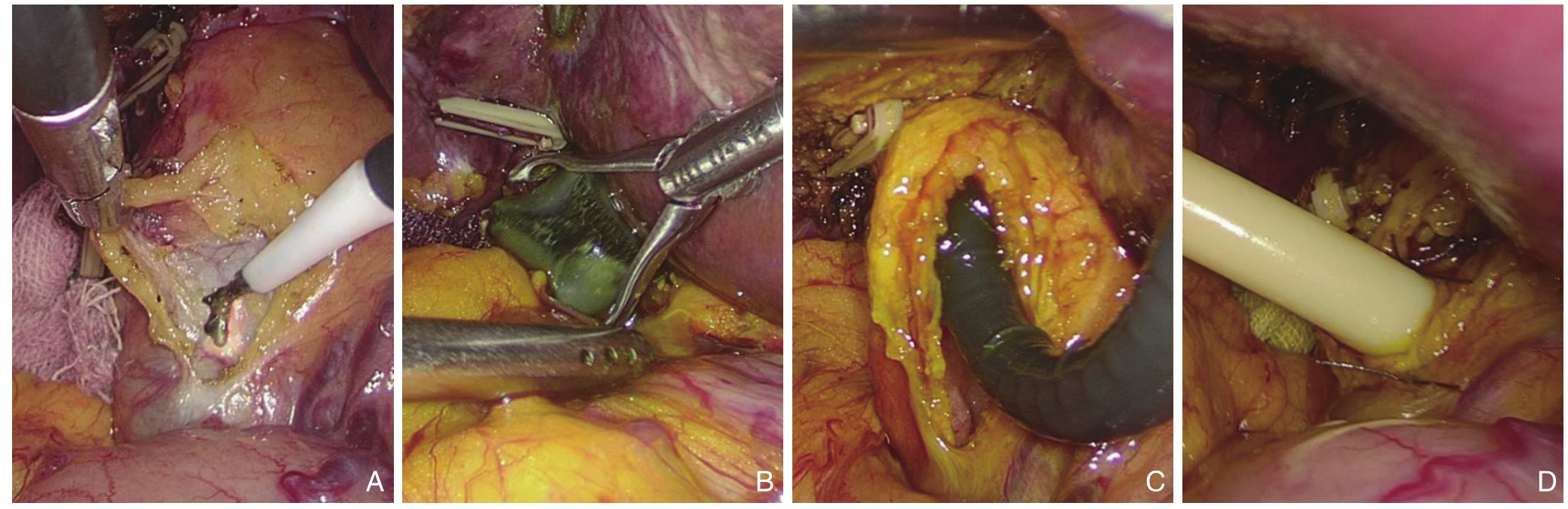
图2 LC+LCBDE组术中图片 A:切开胆总管;B:取出胆总管结石;C:胆道镜检查;D:安置T管并缝合胆管壁
Figure 2 Intraoperative view of the LC+LCBDE group A: Incision of the common bile duct; B: Extraction of the stones in the common bile duct; C: Choledochoscopic exploration of the common bile duct; D: Placement of the T-tube in the bile duct and then choledochal closure
1.3 术后处理
LC+IOERCP组:术后继续禁食,手术后次日行血尿淀粉酶检查,同时观察有无腹痛及腹部体征。如无ERCP术后胰腺炎,嘱患者下床活动并进半流质饮食。若出现ERCP相关并发症,按相应原则进行处理。术后第4天复查血常规及肝肾功能,并经鼻胆管行胆道造影,若无结石残余,肝功能基本恢复正常,可拔除鼻胆管后于第5天出院。
LC+LCBDE组:术后当天禁食,术后次日可下床活动并进半流质饮食。若出现腹腔镜术后相关并发症,按相应原则进行处理。术后1周复查腹部超声后拔除腹腔引流管,保留T管出院。
1.4 观察指标
手术过程的指标:⑴ 中转手术率;⑵ 术中出血量;⑶ 手术总时间;⑷ 结石残余率。术后并发症:⑴ 术后急性胰腺炎或高淀粉酶血症;⑵ 术后出血(包含ERCP术后出血);⑶ 胆汁漏;⑷ 总并发症率。术后平均住院日和住院总费用。
1.5 统计学处理
采用SPSS 18.0统计软件进行统计分析,计量资料以均数±标准差( ±s)表示,采用t检验;计数资料以例数(百分比)[n(%)]表示,采用χ2检验或Fisher精确检验。P<0.05为差异有统计学意义。
±s)表示,采用t检验;计数资料以例数(百分比)[n(%)]表示,采用χ2检验或Fisher精确检验。P<0.05为差异有统计学意义。
2 结 果
2.1 两组患者基线资料比较
LC+IOERCP组42例,男20例,女22例;年龄60~78岁,平均年龄68.5岁;42例患者均有上腹疼痛病史;31例伴有黄疸,3例伴有胆源性胰腺炎;合并有慢性阻塞性肺疾病、糖尿病、高血压病等基础疾病22例。LC+LCBDE组40例,男21例,女19例;年龄60~80岁,平均年龄69.1岁;40例患者均有上腹痛病史;29例伴有黄疸,4例有胆源性胰腺炎;合并基础疾病22例。两组的平均年龄、性别组成及平均病程之间差异无统计学意义(均P>0.05)。两组间总胆红素(TBIL)、谷丙转氨酶(ALT)、谷氨酰转肽酶(GGT)、胆总管直径及最大结石直径之间差异无统计学意义(均P>0.05)(表1)。
表1 两组患者一般临床资料比较
Table 1 Comparison of the general data between the two groups of patients
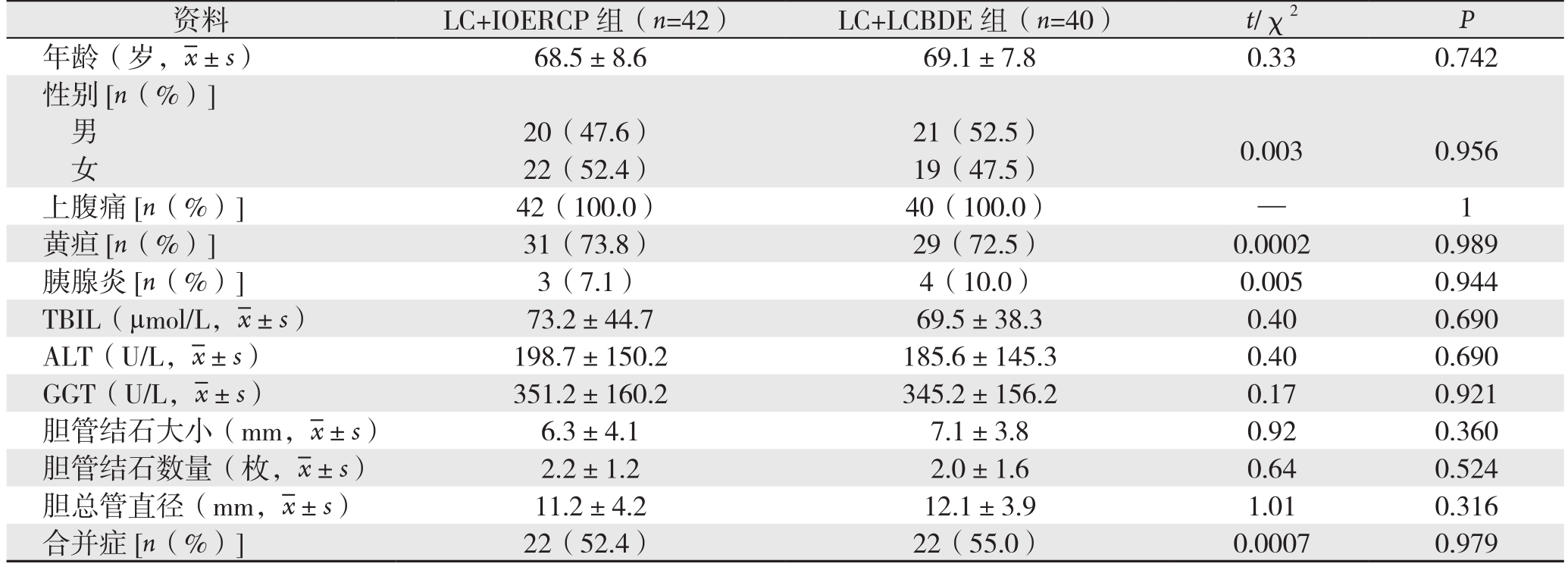
资料 LC+IOERCP组(n=42) LC+LCBDE组(n=40) t/χ2 P年龄(岁, ±s) 68.5±8.6 69.1±7.8 0.33 0.742性别[n(%)]男20(47.6) 21(52.5) 0.003 0.956女22(52.4) 19(47.5)上腹痛[n(%)] 42(100.0) 40(100.0) — 1黄疸[n(%)] 31(73.8) 29(72.5) 0.0002 0.989胰腺炎[n(%)] 3(7.1) 4(10.0) 0.005 0.944 TBIL(µmol/L,
±s) 68.5±8.6 69.1±7.8 0.33 0.742性别[n(%)]男20(47.6) 21(52.5) 0.003 0.956女22(52.4) 19(47.5)上腹痛[n(%)] 42(100.0) 40(100.0) — 1黄疸[n(%)] 31(73.8) 29(72.5) 0.0002 0.989胰腺炎[n(%)] 3(7.1) 4(10.0) 0.005 0.944 TBIL(µmol/L, ±s) 73.2±44.7 69.5±38.3 0.40 0.690 ALT(U/L,
±s) 73.2±44.7 69.5±38.3 0.40 0.690 ALT(U/L, ±s) 198.7±150.2 185.6±145.3 0.40 0.690 GGT(U/L,
±s) 198.7±150.2 185.6±145.3 0.40 0.690 GGT(U/L, ±s) 351.2±160.2 345.2±156.2 0.17 0.921胆管结石大小(mm,
±s) 351.2±160.2 345.2±156.2 0.17 0.921胆管结石大小(mm, ±s) 6.3±4.1 7.1±3.8 0.92 0.360胆管结石数量(枚,
±s) 6.3±4.1 7.1±3.8 0.92 0.360胆管结石数量(枚, ±s) 2.2±1.2 2.0±1.6 0.64 0.524胆总管直径(mm,
±s) 2.2±1.2 2.0±1.6 0.64 0.524胆总管直径(mm, ±s) 11.2±4.2 12.1±3.9 1.01 0.316合并症[n(%)] 22(52.4) 22(55.0) 0.0007 0.979
±s) 11.2±4.2 12.1±3.9 1.01 0.316合并症[n(%)] 22(52.4) 22(55.0) 0.0007 0.979
2.2 两组患者手术相关指标及术后并发症比较
LC+IOERCP组有2例ERCP不成功而中转为腹腔镜胆总管探查取石,手术成功率95.24%(40/42),有1例出现十二指肠乳头切口出血,有1例出现术后高淀粉酶血症,40例均无结石残留;LC+LCBDE组有1例因胆囊三角区粘连致密而中转开腹手术,成功率97.5%(39/40),有1例出现术后腹腔出血,有1例胆汁漏,有6例胆管结石残留。两组中均无医源性消化道穿孔、严重腹膜后感染及死亡病例。两组手术时间、术中出血量及中转手术率,差异均无统计学意义(均P>0.05);LC+IOERCP组结石残留率为0,LC+LCBDE组为15.4%,差异有统计学意义(P<0.05);两组间各并发症及总并发症率之间差异均无统计学意义(P>0.05)(表2)。
表2 两组手术相关指标及术后并发症比较
Table 2 Comparison of the relevant surgical variables and postoperative complications between the two groups
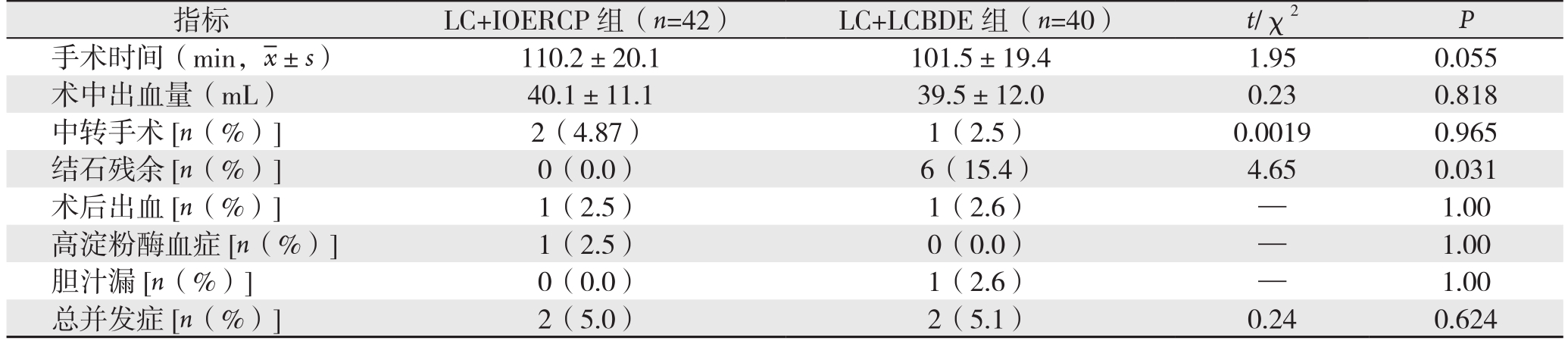
指标 LC+IOERCP组(n=42) LC+LCBDE组(n=40) t/χ2 P手术时间(min, ±s) 110.2±20.1 101.5±19.4 1.95 0.055术中出血量(mL) 40.1±11.1 39.5±12.0 0.23 0.818中转手术[n(%)] 2(4.87) 1(2.5) 0.0019 0.965结石残余[n(%)] 0(0.0) 6(15.4) 4.65 0.031术后出血[n(%)] 1(2.5) 1(2.6) — 1.00高淀粉酶血症[n(%)] 1(2.5) 0(0.0) — 1.00胆汁漏[n(%)] 0(0.0) 1(2.6) — 1.00总并发症[n(%)] 2(5.0) 2(5.1) 0.24 0.624
±s) 110.2±20.1 101.5±19.4 1.95 0.055术中出血量(mL) 40.1±11.1 39.5±12.0 0.23 0.818中转手术[n(%)] 2(4.87) 1(2.5) 0.0019 0.965结石残余[n(%)] 0(0.0) 6(15.4) 4.65 0.031术后出血[n(%)] 1(2.5) 1(2.6) — 1.00高淀粉酶血症[n(%)] 1(2.5) 0(0.0) — 1.00胆汁漏[n(%)] 0(0.0) 1(2.6) — 1.00总并发症[n(%)] 2(5.0) 2(5.1) 0.24 0.624
2.3 两组患者总住院费用及术后平均住院时间比较
LC+IOERCP组平均住院费用(24 065.4±1 582.5)元,术后平均住院日(4.0±2.2)d;LC+LCBDE组平均住院费用(20 057.4±1 782.5)元,术后平均住院日(5.8±3.2)d。两组间总住院费用与术后平均住院时间差异均有统计学意义(均P<0.05)(表3)。
表3 两组总住院费用及术后平均住院时间比较( ±s)
±s)
Table 3 Comparison of the hospitalization costs and length of postoperative hospital stay between the two groups( ±s)
±s)
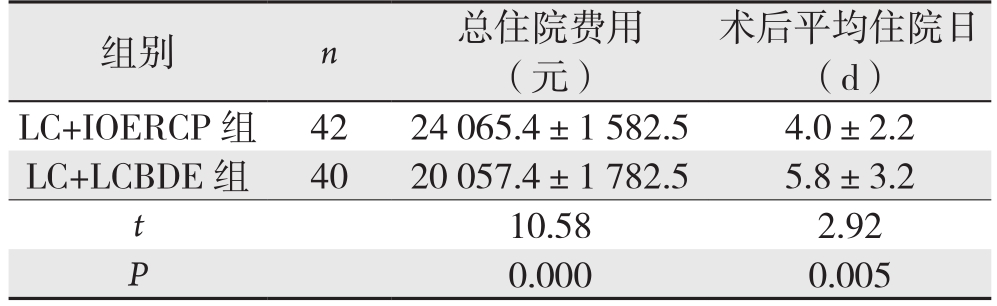
组别 n 总住院费用(元)术后平均住院日(d)LC+IOERCP 组 42 24 065.4±1 582.5 4.0±2.2 LC+LCBDE组 40 20 057.4±1 782.5 5.8±3.2 t 10.58 2.92 P 0.000 0.005
3 讨 论
胆囊结石合并胆总管结石传统的手术治疗方案是开腹胆囊切除及胆总管探查取石,创伤大,恢复慢,且需长期带T管。老年患者病情复杂,器官功能衰退,多伴有合并症,手术耐受能力差,手术风险相对较高[8-11]。随着腹腔镜及内镜技术的成熟,目前多采用多镜联合的微创手术方式,其中应用最广泛的是LC+LCBDE和分期LC+ERCP,前者一次手术解决两个问题,但因胆管一期缝合有一定的限制常需长期留置T管,且对胆总管不扩张的患者相对困难;后者无需留置T管,但需分两次手术,患者遭受两次痛苦,住院时间相应延长[9, 11-13]。目前国内外有学者采用LC+IOERCP方式,取得了很好的效果,一次性手术,同时也避免长期安置T管,缩短了住院时间。本研究结果显示,LC+IOERCP与LC+LCBDE比较在手术时间、术中出血量、中转手术率及总并发症率等方面无统计学差异,且结石残余率更低,住院时间更短,说明老年患者行LC+IOERCP是安全有效的,更具有微创意义。张国强等[7]手术方法与本研究相似,只是没有分年龄阶段,其平均年龄(56.5±12.4)岁,其他如结石大小及结石数量、胆管直径等方面与本研究相似,其结石残余率为0,高淀粉酶血症率为4%,术后住院时间(5.1±1.0)d,与本研究对比无明显差异,因此,笔者认为老年患者行LC+IOERCP与其他患者一样安全有效。
LC联合IOERCP在LC与ERCP先后顺序上有3种方式,⑴ 先侧卧或俯卧行ERCP取石,再变换成仰卧位行LC;⑵ 先仰卧位行LC,再侧卧或俯卧行ERCP取石;⑶ LERV:经胆囊管将导丝插入十二指肠,十二指肠镜下拉出导丝,顺导丝插入附件,进行切开取石操作[14]。先行ERCP可导致肠道充气严重而影响腹腔镜的操作,增加手术时间及风险。先行LC可以避免肠道积气的情况,但仍需改变体位,同时会面临ERCP失败中转腹腔镜胆道探查而需再次改变体位、重新消毒、重新建立气腹等情况的尴尬。这两种情况ERCP均是常规插管,仍有诱发胰腺炎的风险以及ERCP失败的可能。Feretis等[15]于1994年首先完成腹腔镜内镜会师技术,该技术提高了ERCP插管成功率,减少插管次数、缩短了插管时间、避免了插入胰管的可能从而降低ERCP后胰腺炎的发生机率,也减少了内镜操作的时间[7,16-20]。同时,LERV操作时常规作术中胆道造影了解胆管结石情况,可以避免因结石排出[21]而进行的阴性胆道探查或不必要的ERCP[22]。LERV在操作过程中仍然有肠道充气的情况,笔者在手术流程上做了改进,在腹腔镜操作过程中,先把胆囊动脉处理后,暂不处理胆囊管,把胆囊完全剥离并把胆囊床做相应的处理,最后再钳夹胆囊管远端,近端剪开而不剪断,插入弓形刀及导丝进入胆总管,不剪断胆囊管的目的是用胆囊作为牵引,便于胆囊管插入弓形刀及导丝。另外在导丝引导弓形刀从乳头插入胆管交换导丝后,把腹腔镜剩余操作做完,再完成ERCP操作。这样改进过后,把ERCP前腹腔镜的操作大部分完成,最大限度的减少了肠道充气对腹腔镜的操作的影响。LERV操作过程中也存在一些困难,因为采用仰卧位,ERCP操作会存在困难[20],需要极度右旋镜身,并且有时需要右旋小旋钮并锁死,才能得到比较满意的乳头插管位置;平卧位时十二指肠降段处于相对低位,消化液容易在此集聚,影响操作的视野;在有些如结石嵌顿于胆管下端、乳头结构变异等情况,导丝不能通过乳头插入十二指肠肠腔而导致手术失败。本组均采用LERV完成,插管成功率95.24%(40/42),1例因胆管结石嵌顿于胆管下端而失败,另外1例因乳头解剖结构变异,导丝无法通过乳头而失败。急性胰腺炎是ERCP术后最常见的并发症,文献[23]报道发生率为1.6%~13.3%,全组无ERCP术后胰腺炎的发生,仅1例出现高淀粉酶血症。
本研究中LC联合IOERCP组无胆管残余结石,相较LC+LCBDE组差异有统计学意义(P<0.05)。LCDBE术中使用胆道镜取石,因戳孔位置与胆总管成角的原因,部分结石在胆道镜检查过程中可能遗漏,造成残余结石,需等待6~8周后再次经窦道行胆道镜取石,给患者带来不便和痛苦。而LC联合术中ERCP组先行LC术,操作时先夹闭胆囊管,避免了结石掉入胆管,再通过十二指肠镜取石球囊及取石网篮取出胆管内结石,造影确认无结石残余后才完成手术,可充分避免结石残余。
在临床工作中发现,有部分胆囊结石合并胆总管结石患者为继发性胆总管结石,这类患者胆总管一般扩张不明显,部分患者胆总管直径甚至≤8 mm。对于胆管不扩张的患者行LCBDE时,手术相对困难,而且有发生术后胆管狭窄可能。有很多学者[24]认为,为了避免胆管狭窄,胆总管直径≤8 mm时,建议选用ERCP取石,也有些学者[25-26]建议胆管直径≤10 mm时首选ERCP取石。本研究中9例患者胆管直径均对≤8 mm,术中ERCP组6例,LCBDE组3例,发现这些患者在做胆道探查手术时间更长,安置T管缝合胆管更困难。术后随访中还未发现胆管狭窄者。对胆管直径仅有5~6 mm患者,未尝试胆道探查,直接选择行ERCP取石。笔者认为对于胆管直径不扩张的患者LC联合IOERCP的方法治疗更有优势。
老年患者一般合并有较多基础疾病,有些患者心肺功能差而不能耐受麻醉和气腹,且老年患者胆总管结石病情发展迅速,胆管炎症重,一般状况差,因此很多老年患者不适宜作同期手术。笔者对以下几种情况的老年胆囊结石合并胆总管结石患者不做同期手术:⑴ 基础疾病严重、心肺功能差不能耐受全身麻醉患者;⑵ 胆管炎症较重的患者;⑶ 合并有重症急性胆源性胰腺炎患者;⑷ 合并轻型胆源性胰腺炎,但胆道梗阻明显者。
总之,LC联合IOERCP同期治疗老年胆囊结石合并胆总管结石是安全有效的,更具备恢复快、住院时间短,不需长期带T管等优点;应用腹腔镜内镜会师技术,能显著降低ERCP术后胰腺炎的发生率和结石残余率。
[1]Dasari BV, Tan CJ, Gurusamy KS, et al. Surgical versus endoscopic treatment of bile duct stones[J]. Cochrane Database Syst Rev, 2013,(12):CD003327. doi: 10.1002/14651858.CD003327.
[2]Noble H, Tranter S, Chesworth T, et al. A randomized, clinical trial to compare endoscopic sphincterotomy and subsequent laparoscopic cholecystectomy with primary laparoscopic bile duct exploration during cholecystectomy in higher risk patients with choledocholithiasis[J]. J Laparoendosc Adv Surg Tech A, 2009,19(6):713–720. doi: 10.1089/lap.2008.0428.
[3]Ghazal AH, Sorour MA, El-Riwini M, et al. Single-step treatment of gall-bladder and bile duct stones: A combined endoscopic–laparoscopic technique[J]. Int J Surg, 2009, 7(4):338–346. doi:10.1016/j.ijsu.2009.05.005.
[4]Rábago LR, Ortega A, Chico I, et al. Intraoperative ERCP: What role does it have in the era of laparoscopic cholecystectomy?[J].World J Gastrointest Endosc, 2011, 3(12):248–255. doi: 10.4253/wjge.v3.i12.248.
[5]EI Nakeeb A, Sultan AM, Hamdy E, et al. Intraoperative endoscopic retrograde cholangio-pancreatography: a useful tool in the hands of the hepatobiliary surgeon[J]. World J Gastroenterol, 2015,21(2):609–615. doi: 10.3748/wjg.v21.i2.609.
[6]吴君正, 许晓飞, 刘浩, 等. 腹腔镜联合十二指肠镜同期治疗胆囊结石并肝外型肝胆管结石[J]. 南方医科大学学报, 2013,33(11):1656–1660. doi: 10.3969/j.issn.1673–4254.2013.11.20.Wu JZ, Xu XF, Liu H, et al. Combined endoscopiclaparoscopic techniques for one-stage treatment of concomitant cholelithiasis and choledocholithiasis[J]. Journal of Southern Medical University, 2013, 33(11):1656–1660. doi: 10.3969/j.issn.1673–4254.2013.11.20.
[7]张国强, 冯雪峰, 金燕平, 等. 腹腔镜胆囊切除联合术中与术前内镜十二指肠乳头括约肌切开治疗胆石症[J]. 中华肝胆外科杂志, 2015, 21(4):248–252. doi:10.3760/cma.j.issn.1007–8118.2015.04.009.Zhang GQ, Feng XF, Jin YP, et al. Laparoscopic cholecystectomy combined with intraoperative versus preoperative endoscopic sphincterotomy in the treatment of cholecystocholedocholithiasis[J].Chinese Journal of Hepatobiliary Surgery, 2015, 21(4):248–252. doi:10.3760/cma.j.issn.1007–8118.2015.04.009.
[8]梁阔, 刘东斌, 刘家峰, 等. 腹腔镜胆总管探查一期缝合治疗老年胆总管结石的临床疗效分析[J]. 中国普通外科杂志, 2017,26(8):1030–1035. doi:10.3978/j.issn.1005–6947.2017.08.011.Liang K, Liu DB, Liu JF, et al. Clinical efficacy of laparoscopic common bile duct exploration with primary closure for choledocholithiasis in elderly patients[J]. Chinese Journal of General Surgery, 2017, 26(8):1030–1035. doi:10.3978/j.issn.1005–6947.2017.08.011.
[9]王中魁, 赵海鹰, 刘金钢, 等. 老年人胆囊结石合并胆总管结石术式选择探讨[J]. 中国实用外科杂志, 2015, 35(4):448–450.Wang ZK, Zhao HY, Liu JG, et al. Comparison of operative methods for older patients with concomitant cholelithiasis and choledocholithiasis:A report of 60 patients[J]. Chinese Journal of Practical Surgery, 2015, 35(4):448–450.
[10]赵云, 杨成林, 冯以斌, 等. 十二指肠镜联合腹腔镜治疗老年胆囊结石合并肝外胆管结石[J]. 中国普通外科杂志, 2016,25(8):1105–1111. doi:10.3978/j.issn.1005–6947.2016.08.003.Zhao Y, Yang CL, Feng YB, et al. Therapeutic combined use of duodenoscopy and laparoscopy for elderly patients with gallbladder stones and concomitant extrahepatic bile duct stones[J]. Chinese Journal of General Surgery, 2016, 25(8):1105–1111. doi:10.3978/j.issn.1005–6947.2016.08.003.
[11]蒋亚新, 季德刚, 马宁, 等. 两种微创术式治疗老年胆囊结石合并胆总管结石的临床对比[J]. 中国普通外科杂志, 2017, 26(2):139–144. doi:10.3978/j.issn.1005–6947.2017.02.002.Jiang YX, Ji DG, Ma N, et al. Clinical comparison of two minimally invasive procedures for cholecystolithiasis with choledocholithiasis in elderly patients[J]. Chinese Journal of General Surgery, 2017,26(2):139–144. doi:10.3978/j.issn.1005–6947.2017.02.002.
[12]李宇, 郝杰, 孙昊, 等. 一期腹腔镜胆囊切除联合胆总管探查取石与分期内镜取石和腹腔镜胆囊切除术治疗胆囊结石合并胆总管结石的比较[J]. 中国普通外科杂志, 2016, 25(2):202–208.doi:10.3978/j.issn.1005–6947.2016.02.008.Li Y, Hao J, Sun H, et al. One-staged laparoscopic cholecystectomy and common bile duct exploration versus two-staged endoscopic stone extraction followed by laparoscopic cholecystectomy for concomitant cholecystolithiasis and choledocholithiasis [J]. Chinese Journal of General Surgery, 2016, 25(2):202–208. doi:10.3978/j.issn.1005–6947.2016.02.008.
[13]Al-Temimi MH, Kim EG, Chandrasekaran B, et al. Laparoscopic common bile duct exploration versus endoscopic retrograde cholangiopancreatography for choledocholithiasis found at time of laparoscopic cholecystectomy: Analysis of a large integrated health care system database[J]. Am J Surg, 2017, 214(6):1075–1079. doi:10.1016/j.amjsurg.2017.08.030.
[14]Dumange Chapuis-Roux E, Allart K, Delcenserie R, et al. Singlestage management of cholelithiasis and choledocholithiasis:Laparoscopic cholecystectomy and intra-operative endoscopic sphincterotomy (with video) [J]. J Visc Surg, 2018, pii: S1878–7886(18)30036–5. doi: 10.1016/j.jviscsurg.2018.03.011. [Epub ahead of print]
[15]Feretis C, Kalliakmanis B, Benakis P, et al. Laparoscopic transcystic papillotomy under endoscopic control for bile duct stones[J].Endoscopy, 1994, 26(8):697–700. doi: 10.1055/s-2007–1009068.
[16]Vettoretto N, Arezzo A, Famiglietti F, et al. Laparoscopicendoscopic rendezvous versus preoperative endoscopic sphincterotomy in people undergoing laparoscopic cholecystectomy for stones in the gallbladder and bile duct [J]. Cochrane Database Syst Rev, 2018, 4:CD010507. doi: 10.1002/14651858.CD010507.
[17]La Barba G, Gardini A, Cavargini E,et al. Laparoendoscopic rendezvous in the treatment of cholecysto-choledocholitiasis: a single series of 200 patients[J]. Surg Endosc, 2018, 32(9):3868–3873. doi: 10.1007/s00464–018–6125–0.
[18]Tsiopoulos F, Kapsoritakis A, Psychos A, et al. Laparoendoscopic rendezvous may be an effective alternative to a failed preoperative endoscopic retrograde cholangiopancreatography in patients with ch olecystocholedocholithiasis[J]. Ann Gastroenterol, 2018, 31(1):102–108. doi: 10.20524/aog.2017.0210.
[19]Tarantino G, Magistri P, Ballarin R,et al. Surgery in biliary lithiasis: from the traditional "open" approach to laparoscopy and the "rendezvous" technique[J]. Hepatobiliary Pancreat Dis Int,2017, 16(6):595–601. doi: 10.1016/S1499–3872(17)60031–6.
[20]La Greca G, Barbagallo F, Sofia M, et al. Simultaneous laparoendoscopic rendezvous for the treatment of cholecystochole docholithiasis[J]. Surg Endosc, 2009, 24(4):769–780. doi: 10.1007/s00464–009–0680–3.
[21]张奇, 孙备. 梗阻型胆源性胰腺炎内镜治疗时机的选择[J]. 中国普通外科杂志, 2008, 17(3):203–206. doi:10.3969/j.issn.1005–6947.2008.03.001.Zhang Q, Sun B. The timing of endoscopic therapy of obstructive acute biliary pancreatitis[J]. Chinese Journal of General Surgery,2008, 17(3):203–206. doi:10.3969/j.issn.1005–6947.2008.03.001.
[22]Rizzuto A, Fabozzi M, Settembre A, et al. Intraoperative cholangiography during cholecystectomy in sequential treatment of cholecystocholedocholithiasis: To be, or not to be, that is the question A cohort study[J]. Int J Surg, 2018, 53:53–58. doi: 10.1016/j.ijsu.2018.03.023.
[23]Choi YH, Jang DK, Lee SH, et al. Utility of serum phosphate as a marker for predicting the severity of post-endoscopic retrograde cholangiopancreatography pancreatitis[J].United European Gastroenterol J, 2018, 6(6):895–901. doi:10.1177/2050640618764168.
[24]黄三雄, 吴育连, 唐成武, 等. 两种不同微创方法治疗老年胆囊结石合并胆总管结石的疗效对比[J]. 中国老年学杂志, 2014,34(24):6930–6932. doi:10.3969/j.issn.1005–9202.2014.24.038.Huang SX, Wu YL, Tang CW, et al. Comparison of two different minimal invasive methods in treatment of concomitant cholelithiasis and choledocholithiasis in elderly patients[J]. Chinese Journal of Gerontology, 2014, 34(24):6930–6932. doi:10.3969/j.issn.1005–9202.2014.24.038.
[25]游蓁, 叶辉, 熊先泽, 等. LC+LCBDE与ERCP/EST+LC治疗胆囊结石合并胆总管结石的梗阻性黄疸患者的临床对照研究[J]. 中国普外基础与临床杂志, 2013, 20(11):1268–1271.You Z, Ye H, Xiong XZ, et al. Clinical Comparative Analysis of LC+LCBDE and ERCP/EST+LC for CholecystoUthiasis with Choledocholithiasis Patients with Obstructive Jaundice[J].Chinese Journal of Bases and Clinics In General Surgery, 2013,20(11):1268–1271.
[26]徐浩, 孙举来, 芮翾, 等. 胆囊结石合并胆总管结石的微创治疗体会[J]. 腹腔镜外科杂志, 2017, 22(5):352–355. doi:10.13499/j.cnki.fqjwkzz.2017.05.352.Xu H, Sun JL, Rui X, et al. Clinical trials of the efficiency of miniinvasive treatment for cholecystolithiasis and choledocholithiasis[J].Journal of Laparoscopic Surgery, 2017, 22(5):352–355.doi:10.13499/j.cnki.fqjwkzz.2017.05.352.