腹腔镜下胆囊切除术(laparoscopic cholecystectomy,LC)为临床治疗多种胆囊疾病的常见术式,具有微创、术后并发症少和术后恢复快等优点,但手术仍然存在痛感,围手术期合理选择麻醉方式也是确保手术效果的关键。研究[1]发现,使用复合短效麻醉镇痛药物有助于减少患者术后疼痛,稳定围手术期血流动力学指标和应激反应。舒芬太尼与瑞芬太尼是腹腔镜手术常用的与丙泊酚联用的麻醉镇痛药[2-3],但两者的麻醉效果仍有较大争议,如于秀青[4]认为与舒芬太尼比,瑞芬太尼联合丙泊酚麻醉在腹腔镜手术麻醉,缩短患者恢复自主呼吸,稳定术中生命体征平稳及降低术后不良反应,但武长君等[5]认为与瑞芬太尼比,舒芬太尼复合丙泊酚在腹腔镜术中的效果更好,血流动力学及应激反应更平稳,陈晓宇等[6]认为舒芬太尼更适用于老年患者。基于此,本研究将舒芬太尼复合丙泊酚用于LC,观察并比较舒芬太尼与瑞芬太尼麻醉效果,现报告如下。
1 资料与方法
1.1 一般资料
选取2017年3月—2018年3月在我院确诊因胆囊病变择期行LC的90例患者作为研究对象[7]。纳入标准:⑴ 年龄25~68岁;⑵ 美国麻醉师协会(American Society of Anesthesiologists,ASA)分级I~II级;⑶ 体质量指数20~30 kg/m2;⑷ 均无腹部手术史;⑸ 患者对本研究知情同意,签署知情同意书;⑹ 本研究经医院伦理委员会讨论,批准同意。排除标准:⑴ 合并精神障碍疾病患者;⑵ 严重肝肾功能不全患者;⑶ 对本研究麻醉药物过敏患者;⑷ 术中失血过多,严重影响血流动力学指标患者。根据随机数字表法将患者分为两组,每组各45例。一组采用舒芬太尼复合丙泊酚麻醉(舒芬太尼组),其中男27例,女18例;年龄25~65岁,平均年龄(41.36±8.58)岁;体质量43~77 kg,平均(58.12±5.33)kg;手术时间平均(53.58±11.37)min;疾病类型:结石性胆囊炎37例,胆囊息肉5例,其他3例。另一组采用瑞芬太尼复合丙泊酚麻醉(瑞芬太尼组),其中男25例,女20例;年龄26~68岁,平均年龄(42.18±8.93)岁;体质量42~75 kg,平均(57.37±5.65)kg;手术时间平均(52.15±10.68)min;疾病类型:结石性胆囊炎36例,胆囊息肉6例,其他3例。两组患者一般临床资料比较无统计学差异(均P>0.05),有可比性。
1.2 方法
患者术前均常规禁食禁饮,两组均实施LC,术前30 min给予0.5 mg阿托品、0.1 g苯巴比妥肌肉注射。入室后常规开放静脉通道,监测心率(HR)、血氧饱和度(SpO2)、心电图、血压。面罩吸氧,麻醉诱导阶段,给予咪达唑仑(江苏恩华药业股份有限公司,规格10 mg/2 mL,国药准字:H20031037)0.02~0.04 mg/kg,丙泊酚(西安力邦制药有限公司,规格200 mg/20 mL,国药准字:H19990282)1~2 mg/kg,舒芬太尼(宜昌人福药业有限责任公司,规格100 μg /1 mL,国药准字:H20054172)0.4~0.6 µg/kg,顺阿曲库铵(江苏恒瑞医药股份有限公司,规格10 mg/支,国药准字:20060869)0.15 mg/kg。
麻醉诱导后行气管插管全身麻醉。麻醉维持阶段:舒芬太尼组给予舒芬太尼0.2~0.4 μg/(kg·h),丙泊酚4~6 mg/(kg·h),根据手术实际情况给予顺阿曲库铵0.1 mg/kg间断注射维持肌松至手术结束。瑞芬太尼组给予瑞芬太尼(国药集团工业有限公司廊坊分公司,规格1 mg,国药集团工业有限公司廊坊分公司)0.15 μg/(kg·min),丙泊酚4~6 mg/(kg·h),并根据手术情况给予顺阿曲库铵0.1 mg/kg维持肌松至手术结束。
1.3 观察指标
⑴ 记录两组麻醉诱导前(T0)、麻醉诱导气管插管即刻(T1)、CO2气腹后5 min(T2)、拔管即刻(T3)和拔管后10 min(T4)的血流动力学指标变化与血清应激指标,前者包括平均动脉压(MAP)、HR和SpO2;后者包括患者各时间段血清去甲肾上腺素(NE)和皮质醇(Cor)水平,采用酶联免疫试剂盒检测。⑵记录患者自主呼吸恢复时间、睁眼时间和拔管时间。⑶ 采用视觉模拟评分法(VAS),记录患者术后1、6、12 h的疼痛情况,计分为0~10分,患者根据自身疼痛情况进行判断,分数越高提示疼痛越严重。⑷ 采用简易精神状态量表(MMSE),记录患者术前1 d、术后1、3 d的认知功能,当MMSE≤23分时,提示认知功能障碍。⑸ 统计患者麻醉复苏期并发症发生情况。
1.4 统计学处理
数据处理用SPSS 20.0软件,组间计数资料用例数(百分比)[n(%)]表示,采用χ2检验,若理论频数≤5,采用Fisher确切概率法检验;计量资料用均数±标准差( ±s),比较用方差分析检验,组间两两比较采用SNK检验,P<0.05为差异有统计学意义。
±s),比较用方差分析检验,组间两两比较采用SNK检验,P<0.05为差异有统计学意义。
2 结 果
2.1 两组各时间点的血流动力学指标变化
两组各时间点的SpO2水平比较无统计学差异(均P>0.05),舒芬太尼组T1、T2和T3时间点的MAP和HR较瑞芬太尼组明显降低(均P<0.05),两组T0和T4时间点的MAP和HR比较无统计学差异(均P>0.05)(表1)。
表1 两组各时间点血流动力学指标比较(n=45, ±s)
±s)
Table 1 Comparison of the hemodynamic variables at each time point between the two groups (n=45,  ±s)
±s)

注:1)与瑞芬太尼组比较,P<0.05
Note: 1) P<0.05 vs. remifentanil group
组别 T0 T1 T2 T3 T4 F P舒芬太尼组MAP(p/kPa) 12.31±2.13 13.02±1.101) 11.53±1.671) 12.24±1.351) 12.57±1.41 5.386 0.000 HR(次/min) 78.03±10.58 85.23±12.351) 73.54±10.021) 85.54±7.351) 84.34±7.96 13.247 0.000 SpO2(%) 89.32±8.92 89.51±7.59 89.34±8.85 89.24±7.05 89.35±8.11 0.007 1.000瑞芬太尼组MAP(p/kPa) 12.09±2.24 15.51±1.32 13.81±1.80 14.93±1.41 13.05±1.53 30.059 0.000 HR(次/min) 77.93±9.97 95.37±13.96 77.24±10.20 95.24±12.35 86.37±8.25 28.561 0.000 SpO2(%) 88.21±9.06 89.13±8.85 89.23±9.02 89.59±8.37 89.18±8.57 0.153 0.961
2.2 血清应激指标变化
两组T0时间点的血清Cor和NE水平比较无统计学差异(均P>0.05),舒芬太尼组T1、T2、T3和T4时间点的血清Cor和NE水平均明显低于瑞芬太尼组(均P<0.05)(表2)。
2.3 两组自主呼吸恢复时间、睁眼时间和拔管时间比较
与瑞芬太尼组比较,舒芬太尼组自主呼吸恢复时间、睁眼时间和拔管时间均明显延长(均P<0.05)(表3)。
表2 两组各时间点血清应激指标变化指标比较(ng/mL,n=45, ±s)
±s)
Table 2 Comparison of the serum stress indicators at each time point between the two groups (ng/mL, n=45,  ±s)
±s)
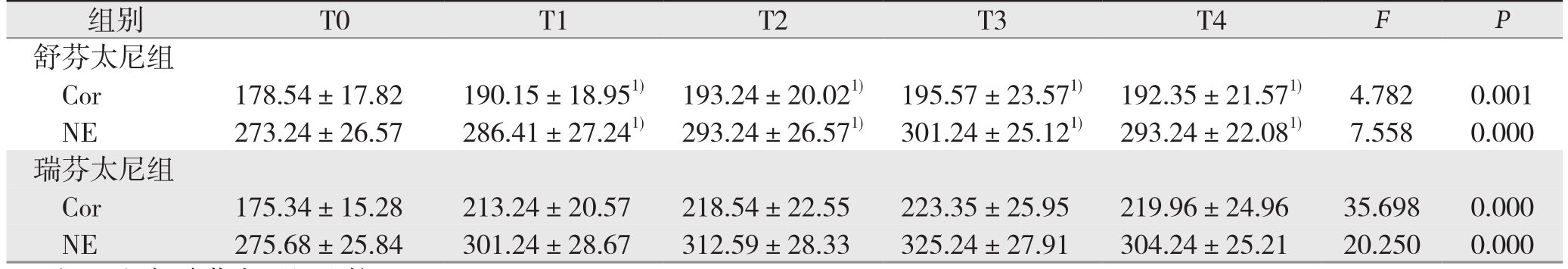
注:1)与瑞芬太尼组比较,P<0.05
Note: 1) P<0.05 vs. remifentanil group
组别 T0 T1 T2 T3 T4 F P舒芬太尼组Cor 178.54±17.82 190.15±18.951) 193.24±20.021) 195.57±23.571) 192.35±21.571) 4.782 0.001 NE 273.24±26.57 286.41±27.241) 293.24±26.571) 301.24±25.121) 293.24±22.081) 7.558 0.000瑞芬太尼组Cor 175.34±15.28 213.24±20.57 218.54±22.55 223.35±25.95 219.96±24.96 35.698 0.000 NE 275.68±25.84 301.24±28.67 312.59±28.33 325.24±27.91 304.24±25.21 20.250 0.000
表3 两组自主呼吸恢复时间、睁眼时间和拔管时间比较对比(min,n=45, ±s)
±s)
Table 3 Comparison of the times to recovery of spontaneous breathing, eye opening and extubation between the two groups (min, n=45,  ±s)
±s)
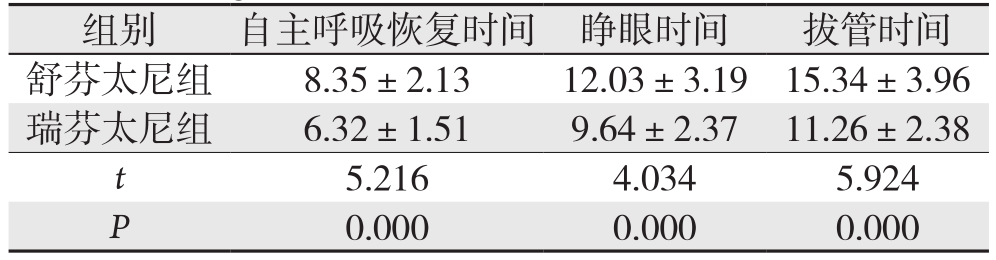
组别 自主呼吸恢复时间 睁眼时间 拔管时间舒芬太尼组 8.35±2.13 12.03±3.19 15.34±3.96瑞芬太尼组 6.32±1.51 9.64±2.37 11.26±2.38 t 5.216 4.034 5.924 P 0.000 0.000 0.000
2.4 两组患者术后各时间段VAS评分比较
与瑞芬太尼组比较,舒芬太尼组术后1、6、12 h的VAS评分均明显降低(均P<0.05)(表4)。
表4 两组患者术后各时间段VAS评分比较(n=45, ±s)
±s)
Table 4 Comparison of the VAS scores at each time point after operation between the two groups (n=45,  ±s)
±s)
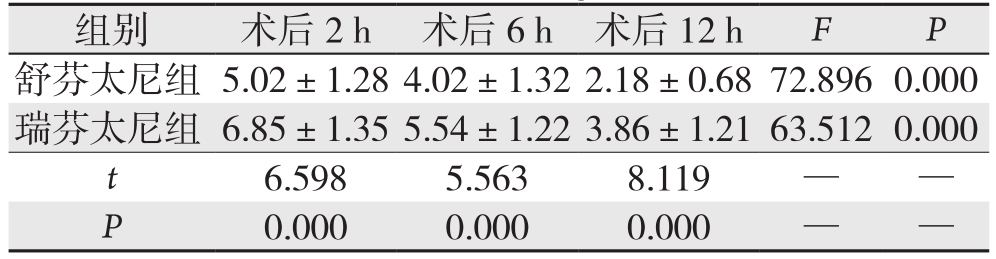
组别 术后2 h 术后6 h 术后12 h F P舒芬太尼组 5.02±1.284.02±1.322.18±0.6872.896 0.000瑞芬太尼组 6.85±1.355.54±1.223.86±1.2163.512 0.000 t 6.5985.5638.119——P 0.0000.0000.000——
2.5 两组各时间段MMSE评分比较
两组术前1 d和术后3 d的MMSE评分比较无统计学差异(均P>0.05),舒芬太尼组术后1 d的MMSE评分明显高于瑞芬太尼组(P<0.05)(表5)。
表5 两组各时间点MMSE评分比较(n=45, ±s)
±s)
Table 5 Comparison of the MMSE scores at each time point between the two groups (n=45,  ±s)
±s)
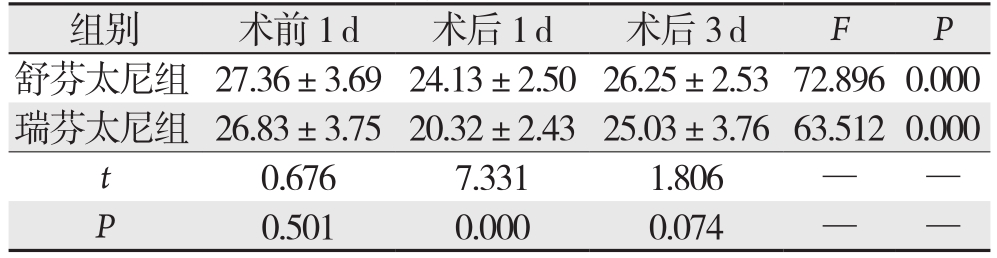
组别 术前1 d 术后1 d 术后3 d F P舒芬太尼组 27.36±3.6924.13±2.5026.25±2.5372.896 0.000瑞芬太尼组 26.83±3.7520.32±2.4325.03±3.7663.512 0.000 t 0.676 7.331 1.806——P 0.501 0.000 0.074——
2.6 两组患者麻醉复苏期不良反应发生率情况比较
与瑞芬太尼组比较,舒芬太尼组麻醉复苏期各项并发症均无统计学差异(均P>0.05),总不良反应发生率明显降低(P<0.05)(表6)。
表6 两组患者麻醉复苏期不良反应发生率情况比较[n=45,n(%)]
Table 6 Comparison of the incidence of adverse reactions between the two groups during anesthesia recovery period [n=45, n (%)]
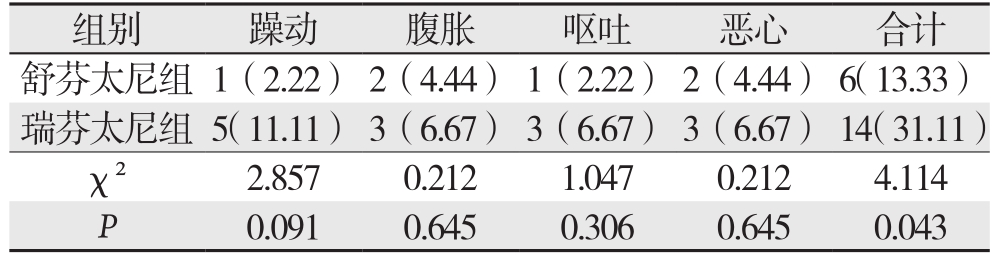
组别 躁动 腹胀 呕吐 恶心 合计舒芬太尼组 1(2.22) 2(4.44) 1(2.22) 2(4.44) 6(13.33)瑞芬太尼组 5(11.11) 3(6.67) 3(6.67) 3(6.67) 14(31.11)χ² 2.857 0.212 1.047 0.212 4.114 P 0.091 0.645 0.306 0.645 0.043
3 讨 论
随着腹腔镜手术的发展,LC也被广泛应用于胆囊结石和胆囊炎等胆囊病变的治疗,虽然腹腔镜手术避免了传统开创性手术带来的巨大创伤,对机体应激反应小,但依旧存在术后疼痛的问题。LC中一般采用气管插管全身麻醉,麻醉期间需要维持足够的麻醉深度,研究发现,合理选择术中麻醉方式对于减轻术中应激反应,降低术后疼痛程度具有重要意义[8]。
LC在全身麻醉时,气管插管操作会引起血液升高,HR加快,且腹腔镜手术中还需要建立CO2气腹,机械操作刺激带来的各种病理性和生理性反应,机体应激可导致血压、心肌收缩功能和HR改变,可能会导致心力衰竭及心律失常等疾病[9],在手术结束后清醒和拔除气管导管期间由于气管内吸引分泌物、伤口疼痛、气管导管留置和拔除等刺激,必然影响到患者血流动力学剧烈变化和应激反应,不利于患者平稳度过麻醉苏醒和恢复期,增加围手术风险[10]。麻醉操作中采用复合麻醉方案,可以减少单一药物用量,药物相关不良反应也会相对减少,麻醉的可控性也更好,还可加快术后恢复,镇痛和肌肉松弛效果更好,更有利于自主神经系统稳定[11]。丙泊酚为一种新型短效麻醉药物,临床常用于全身麻醉的诱导和维持。临床常将瑞芬太尼和瑞芬太尼与丙泊酚联用以改善LC的麻醉效果。
瑞芬太尼为芬太尼类µ型阿片受体激动剂,属于超短效镇痛药物,具有起效快速、半衰期短和代谢快等优点[12]。瑞芬太尼复合丙泊酚麻醉静脉麻醉可降低各自的使用剂量,减少术后并发症和不良反应[13],但在全凭静脉麻醉手术中,手术结束停止用药,患者很快清醒,伤口则疼痛严重。舒芬太尼属于阿片类镇痛药物,是芬太尼N-4位取代的衍生物,属于苯基哌啶类,具有脂溶性高和亲和力高的特点,舒芬太尼与μ受体的结合力较芬太尼高,且为芬太尼的7.7倍[14]。舒芬太尼清除率高[12.7 L/(kg·min)]、清除半衰期短(160 min),舒芬太尼的脂溶性是芬太尼的2倍,与血清中浆蛋白的结合性高,在血浆中的水平较低,再加上舒芬太尼与α-酸性糖蛋白的结合比较疏松,通过注射途径给药后,更容易并快速地分布到各个组织[15],尤其是血脑屏障对该药物的影响小,舒芬太尼容易通过血脑屏障达到脑内并维持有效浓度[16]。如本研究结果显示,给予舒芬太尼的舒芬太尼组围术期T1、T2和T3时间点的MAP和HR升高或波动程度显著低于给予瑞芬太尼的瑞芬太尼组,两组T0和T4时间点的MAP和HR比较统计学差异,各时间点的SpO2比较亦无统计学差异,提示与瑞芬太尼复合丙泊酚比,舒芬太尼复合丙泊酚用于LC麻醉维持对患者血流动力学影响小,该结果与文献[17]报道一致,与舒芬太尼在组织维持有效的血药浓度相关。
NE为一种神经递质,是交感节后神经元和脑内肾上腺素能神经末梢合成和分泌,也是一种激素,在化学结构上也属于儿茶酚胺[5, 18-19];皮质醇为是通过肾上腺皮质线粒体中的11β-羟化酶的作用,由11-脱氧皮质醇生成,其操纵机体情绪、免疫细胞和炎症等[20]。本研究中,舒芬太尼组T1、T2、T3和T4时间点的血清Cor和NE水平均显著低于瑞芬太尼组,提示舒芬太尼复合丙泊酚对患者应激反应小,与舒芬太尼可有效抑制气管插管反应和儿茶酚胺释放相关。本研究中,舒芬太尼组自主呼吸恢复时间、睁眼时间和拔管时间均较瑞芬太尼组显著延长,但舒芬太尼组术后1、6、12 h的VAS评分均显著低于瑞芬太尼组,舒芬太尼组术后1 d的MMSE评分显著高于瑞芬太尼组,提示虽然舒芬太尼复合丙泊酚麻醉较瑞芬太尼复合丙泊酚麻醉自主呼吸恢复时间、苏醒时间和拔管时间延迟,但其镇痛效果更好,镇痛持续时间更长,对患者术后认知障碍影响也更小。两组患者麻醉苏醒期的主要不良反应主要为躁动、腹胀、呕吐和恶心,舒芬太尼组总不良反应发生率(6/45,13.33%)小于瑞芬太尼组(14/45,31.11%),与既往研究[21-25]相符,提示舒芬太尼复合丙泊酚用于LC麻醉镇痛效果好,可减少患者术后躁动、恶心和呕吐等不良反应发生率,更为安全。
综上所述,在LC中,与瑞芬太尼相比,使用舒芬太尼复合丙泊酚静脉麻醉可获得良好的麻醉效果,对患者血流动力学和应激反应小,患者术后疼痛程度轻,对患者认知功能障碍影响小,且还可以减少患者麻醉苏醒期不良反应发生率,有临床推广的价值。
[1]赵晓峥, 张曼, 赵庆阳. 舒芬太尼复合丙泊酚对小面积微创吸脂手术麻醉的效果及安全性评价[J]. 中国药业, 2017, 26(13):69–71.doi:10.3969/j.issn.1006–4931.2017.13.025.Zhao XZ, Zhang M, Zhao QY. Efficacy and Safety of Sufentanil Combined with Propofol on Anesthesia for Small Area Minimally Invasive Liposuction[J]. China Pharmaceuticals, 2017, 26(13):69–71. doi:10.3969/j.issn.1006–4931.2017.13.025.
[2]魏来, 陈文雁, 代亚, 等. 超声引导椎旁神经阻滞对开腹胰十二指肠切除术患者镇痛作用的临床研究[J]. 中国普通外科杂志,2017, 26(9):1174–1179. doi:10.3978/j.issn.1005–6947.2017.09.015.Wei L, Chen WY, Dai Y, et al. Analgesic efficacy of ultrasound guided thoracic paravertebral block in patients undergoing open pancreaticoduodenectomy[J]. Chinese Journal of General Surgery,2017, 26(9):1174–1179. doi:10.3978/j.issn.1005–6947.2017.09.015.
[3]王雷, 袁利刚, 董擂. 瑞芬太尼联合咪达唑仑用于内镜逆行性胆管造影监护性麻醉的效果分析[J]. 中国普通外科杂志, 2016,25(10):1517–1521. doi:10.3978/j.issn.1005–6947.2016.10.025.Wang L, Yuan LG, Dong L. Effect analysis of combined use of remifentanil and midazolam as monitoring anesthetic for endoscopic retrograde cholangiography[J]. Chinese Journal of General Surgery, 2016, 25(10):1517–1521. doi:10.3978/j.issn.1005–6947.2016.10.025.
[4]于秀青. 瑞芬太尼复合丙泊酚与舒芬太尼复合丙泊酚用于腹腔镜下胆囊切除术麻醉效果的比较[J]. 临床合理用药杂志, 2015,8(36):65–66. doi:10.15887/j.cnki.13–1389/r.2015.36.032.Yu XQ. Comparison of effects between remifentanil combined with propofol and sufentanil combined with propofol using in laparoscopic cholecystectomy[J]. Chinese Journal of Clinical Rational Drug Use, 2015, 8(36):65–66. doi:10.15887/j.cnki.13–1389/r.2015.36.032.
[5]武长君, 钱鹏. 舒芬太尼复合丙泊酚对腹腔镜下胆囊切除术患者血流动力学及应激反应的影响[J]. 海南医学院学报, 2014,20(2):273–275.Wu CJ, Qian P. Influence on the sufentanil combined with propofol for the hemodynamics and stress reaction of patients with laparoscopic cholecystectomy[J]. Journal of Hainan Medical University, 2014, 20(2):273–275.
[6]陈晓宇, 王大明, 潘东军, 等. 老年患者腹腔镜下直肠癌手术时异丙酚复合舒芬太尼或瑞芬太尼的对比观察[J]. 新乡医学院学报,2012, 29(9):689–692.Chen XY, Wang DM, Pan DJ, et al. Comparison of the effects of propofol combined with sufentanil or remifentanil anesthesia during laparoscopic surgery for colorectal carcinoma in elderly patients[J].Journal of Xinxiang Medical College, 2012, 29(9):689–692.
[7]Dumange Chapuis-Roux E, Allart K, Delcenserie R, et al. Singlestage management of cholelithiasis and choledocholithiasis:Laparoscopic cholecystectomy and intra-operative endoscopic sphincterotomy (with video)[J]. J Visc Surg, 2018, pii: S1878–7886(18)30036–5. doi: 10.1016/j.jviscsurg.2018.03.011. [Epub ahead of print]
[8]王奎, 付山. 舒芬太尼联合丙泊酚静脉麻醉在腹腔镜胆囊切除术中的麻醉作用研究[J]. 药物评价研究, 2017, 40(2):252–254.doi:10.7501/j.issn.1674–6376.2017.02.023.Wang K, Fu S. Clinical efficacy of Sufentanil combined with propofol in intravenous anesthesia during laparoscopic cholecystectomy[J]. Drug Evaluation Research, 2017, 40(2):252–254. doi:10.7501/j.issn.1674–6376.2017.02.023.
[9]李顺洪, 冯麟, 李林佶, 等. 丙泊酚复合舒芬太尼靶控静脉麻醉对老年肺癌患者术中血流动力学及术后认知功能的影响[J]. 中国老年学杂志, 2017, 37(11):2745–2747. doi:10.3969/j.issn.1005–9202.2017.11.064.Li SH, Feng L, Li LJ, et al. Effect of anesthesia with targetcontrolled infusion of propofol combined with sufentanil on intraoperative hemodynamics and postoperative cognitive function in old patients[J]. Chinese Journal of Gerontology, 2017,37(11):2745–2747. doi:10.3969/j.issn.1005–9202.2017.11.064.
[10]邵伟栋, 张兴安, 刘礼胜, 等. 靶控输注丙泊酚复合舒芬太尼或瑞芬太尼用于肾移植手术的临床研究[J]. 实用医学杂志, 2013,29(20):3331–3333. doi:10.3969/j.issn.1006–5725.2013.20.024.Shao WD, Zhang XA, Liu LS, et al. Target-controlled infusion of sufentanil/propofol versus remifentanil/propofol in patients received renal transplantation[J]. The Journal of Practical Medicine, 2013,29(20):3331–3333. doi:10.3969/j.issn.1006–5725.2013.20.024.
[11]李英杰. 舒芬太尼复合丙泊酚全凭静脉麻醉在神经外科手术中的应用[J]. 中国实用神经疾病杂志, 2015, 18(21):59–60.doi:10.3969/j.issn.1673–5110.2015.21.038.Li YJ. Application of total intravenous anesthesia with sufentanil plus propofol in neurosurgery[J]. Chinese Journal of Practical Nervous Diseases, 2015, 18(21):59–60. doi:10.3969/j.issn.1673–5110.2015.21.038.
[12]谢海玉, 占丽芳, 邓云菱, 等. 丙泊酚复合舒芬太尼靶控静脉麻醉在老年脑外科手术中的应用[J]. 中国老年学杂志, 2012,32(2):281–282. doi:10.3969/j.issn.1005–9202.2012.02.028.Xie HY, Zhan LF, Deng YL, et al. Application of anesthesia with target-controlled infusion of propofol combined with sufentanil in brain surgery for old patients[J]. Chinese Journal of Gerontology,2012, 32(2):281–282. doi:10.3969/j.issn.1005–9202.2012.02.028.
[13]肖维萍, 李铁. 舒芬太尼复合丙泊酚对高血压脑出血手术患者麻醉效果分析[J]. 神经损伤与功能重建, 2015, 10(4):307–308.doi:10.3870/sjsscj.2015.04.009.Xiao WP, Li T. The Anesthesia Efficacy of Sufentanil Combined with Propofol on the Patients with Hypertension Cerebral Hemorrhage Operation[J]. Neural Injury and Functional Reconstruction, 2015, 10(4):307–308. doi:10.3870/sjsscj.2015.04.009.
[14]Modak SD, Kane DG. Conscious sedation for balloon mitral valvotomy: A comparison of fentanyl versus sufentanil[J]. Ann Card Anaesth, 2017, 20(2):163–168. doi:10.4103/0971–9784.203930.
[15]Wilwerth M, Majcher JL, Van der Linden P. Spinal fentanyl vs.sufentanil for post-operative analgesia after C-section: a doubleblinded randomised trial[J]. Acta Anaesthesiol Scand, 2016,60(9):1306–1313. doi: 10.1111/aas.12738.
[16]徐露, 李元海. 舒芬太尼的药理作用和临床应用研究进展[J]. 安徽医药, 2011, 15(3):375–377. doi:10.3969/j.issn.1009–6469.2011.03.051.Xu L, Li YH. Progress of pharmacological actions and clinical applications of sufentanil[J]. Anhui Medical and Pharmaceutical Journal, 2011, 15(3):375–377. doi:10.3969/j.issn.1009–6469.2011.03.051.
[17]赵小飞, 毛婷婷. 脑损伤患者应用芬太尼、瑞芬太尼和舒芬太尼的脑血流动力学比较[J]. 中国医院药学杂志, 2015, 35(4):333–336. doi:10.13286/j.cnki.chinhosppharmacyj.2015.04.15.Zhao XF, Mao TT. Comparative study on cerebral hemodynamics of fentanyl, remifentanil and sufentanil in patients with cerebral injuries[J]. Chinese Journal of Hospital Pharmacy, 2015, 35(4):333–336. doi:10.13286/j.cnki.chinhosppharmacyj.2015.04.15.
[18]Petrosus E, Silva EB, Lay D Jr, et al. Effects of orally administered cortisol and norepinephrine on weanling piglet gut microbial populations and Salmonella passage[J]. J Anim Sci, 2018. doi:10.1093/jas/sky312. [Epub ahead of print]
[19]Wang LY, Raskind MA, Wilkinson CW, et al. Associations between CSF cortisol and CSF norepinephrine in cognitively normal controls and patients with amnestic MCI and AD dementia[J]. Int J Geriatr Psychiatry, 2018, 33(5):763–768. doi: 10.1002/gps.4856.
[20]房建. 右美托咪啶对老年全子宫切除术复合麻醉患者围术期血流动力学和血管应激反应的影响[J]. 中国妇幼保健, 2017, 32(24):6109–6112. doi:10.7620/zgfybj.j.issn.1001–4411.2017.24.17.Fang J. Influences of dexmedetomidine on perioperative hemodynamics and vascular stress response in old patients undergoing hysterectomy with combined anesthesia[J]. Maternal &Child Health Care of China, 2017, 32(24):6109–6112. doi:10.7620/zgfybj.j.issn.1001–4411.2017.24.17.
[21]赵泽宇, 王茜, 张倩, 等. 舒芬太尼复合靶控输注丙泊酚静脉诱导对腹腔镜胆囊切除术老年患者血流动力学的影响[J]. 四川医学,2010, 31(2):152–154. doi:10.3969/j.issn.1004–0501.2010.02.005.Zhao ZY, Wang Q, Zhang Q, et al. Effects of sufentanil combined with target controlled infusion of propofol on hemodynamics in geriattrics with lapacoscopic cholecystectomy during anesthesia induction[J]. Sichuan Medical Journal, 2010, 31(2):152–154.doi:10.3969/j.issn.1004–0501.2010.02.005.
[22]Wang JM, Xu F, Peng G, et al. Efficacy and safety of Sufentanilpropofol versus Remifentanil-propofol as anesthesia in patients undergoing craniotomy: a meta-analysis[J]. World Neurosurg, 2018,pii: S1878–8750(18)31696–6. doi: 10.1016/j.wneu.2018.07.216.[Epub ahead of print]
[23]Luo K, Xu JM, Cao L, et al. Effect of dexmedetomidine combined with sufentanil on preventing emergence agitation in children receiving sevoflurane anesthesia for cleft palate repair surgery[J]. Exp Ther Med, 2017, 14(2):1775–1782. doi: 10.3892/etm.2017.4660.
[24]Zhang Q, Su M. Sufentanil attenuates oxaliplatin cytotoxicity via inhibiting connexin 43-composed gap junction function[J]. Mol Med Rep, 2017, 16(1):943–948. doi: 10.3892/mmr.2017.6669.
[25]Bairy L, Vanderstichelen M, Jamart J, et al. Clonidine or remifentanil for adequate surgical conditions in patients undergoing endoscopic sinus surgery: a randomized study[J]. PeerJ, 2017,5(4):e3370. doi: 10.7717/peerj.3370.