胆囊结石发病率10%~15%,女性多于男性,发病率与年龄成正比。1882年Langenbuch首次行开腹胆囊切除术(open cholecystectomy,OC),1985年Muhe提出腔镜方法,1987年Mouret推行腹腔镜胆囊切除术(laparoscopic cholecystectomy,LC),随后Dubois等[1]提出几个入口的新技术,并总结微创有切口小、影响小、愈合快、住院时间短等优点。从此,LC成为治疗胆囊结石的金标准术式。
美国每年700万例胆囊切除术中70%为腹腔镜手术,而英国更是超过98%,且超过70%是日间手术[2]。在国内,1991年荀祖武首先开展LC,随后LC得到迅速推广,进入21世纪后更是成为首选术式[3]。然而,随着LC的广泛应用,其胆管损伤(bile duct injury,BDI)等并发症引起广泛关注。研究[4-5]表明,LC并发症发生率为0.2%~0.8%是OC的2~4倍,其中BDI发生率为0.1%~0.2%。现就BDI研究现状进行综述。
1 病 因
1.1 解剖因素
后天炎症占BDI的15%~35%,包括炎症所致结痂出血,尤其是合并脂肪过多时;而Calot三角周围炎症增加解剖难度及动脉损伤风险[6-7]。先天异常,其中胆管变异发生率18%~39%,BDI占3%~6%。最常见为变异胆囊管长入肝管,右肝内胆管差异大,尤其Luschka管。右肝动脉异常和胆管伴行异常血管。左位胆囊[6, 8-9]。
1.2 术者经验
误认解剖,胆管误认率达86%,其中70%因低估风险、错误认知和粗心失误,常因不熟悉Calot三角解剖而将胆总管、异位右肝管当作胆囊管钳夹最为常见[10]。错误处理,经验丰富术者也难以修复多数BDI,甚至增加医源性BDI风险[11]。经验瓶颈,经验会达平台期,修复BDI策略需革新[12]。
1.3 仪器因素
⑴ 腹腔镜缺点: 局限于两个面; 缺乏手部触诊;利用正切、低位接近B D I 位置;重大出血中难以观测[6]。⑵ 胆道造影用于明确胆管结石及解剖。是否使用术中胆道造影(intraoperative cholangiography,IOC)意见不一,Beckingham[4]总结有的称减少BDI发生,也有称无任何帮助,更甚称造成超过50% BDI。⑶ 过度使用电灼术解剖Calot三角和周围组织,会增加BDI风险,而超声刀和单极电凝常用于术中解剖、止血,其中超声刀更优[13]。
2 诊 断
2.1 临床表现
常见发热、恶心和腹痛,而阻塞性黄疸后果是残余胆汁引流不畅、胆汁性腹膜炎甚至脓毒性休克[11]。术后胆汁漏(bile duct leakage,BDL)是BDI重要表现,常在术后3~4 d,也可术后30 d[14]。
2.2 检查
2.2.1 解剖 BDI 常发生于胆总管、胆囊管和右肝管。方叶可作解剖Calot 三角的起点,其发育不全易致BDI。右后肝管长入胆总管,而胆囊管与异常肝管间距短,近肝床解剖时易致BDI。BDL 常提示BDI 范围,从小BDL 到完全横断胆管[6, 11]。
2.2.2 影像 影像和血检确认引流管、胆管阻塞引起的黄疸。⑴ 超声和CT:首选超声。均可示液体聚集,引导经皮穿刺引流操作,但难区分胆汁与其他液体。CT 具高空间分辨率,但不能精确定位,增强CT 有所帮助[11, 15]。⑵ 肝胆管描记法:显示功能活动性信息,但空间分辨率差。不提供胆管外解剖,对肝功障碍敏感性差,若BDL 不经十二指肠被误认为完全性胆管堵塞[15]。⑶ 磁共振胰胆管造影(magnetic resonance cholangiopancreatography,MRCP):不具侵袭性被广泛运用,但难检测小漏。运用对比剂评估胆管功能,显示BDL位置,但对比剂在异常肝功能的胆管系统成像欠佳[16]。 ⑷ 内镜逆行胰胆管造影(endoscopic retrograde cholangiopancreatography,ERCP)与经皮肝胆管造影(percutaneous transhepatic cholangiography,PTC):ERCP 可诊断小BDI 指导引流,但难以发现右后叶VI、VII 段BDL,在综合性医疗中心才被优先考虑[17]。PTC 能确定活动性BDL,提供精确解剖、扩张胆管树减压治疗[18]。两者具侵袭性,难检测肝外异常如堵塞(粘连、结石)上下段,使用大量X 线,可引起重症胰腺炎(ERCP)、出血和胆管炎(PTC)等并发症。此外,PTC 还因肝内胆管不扩张而难以实施[19]。
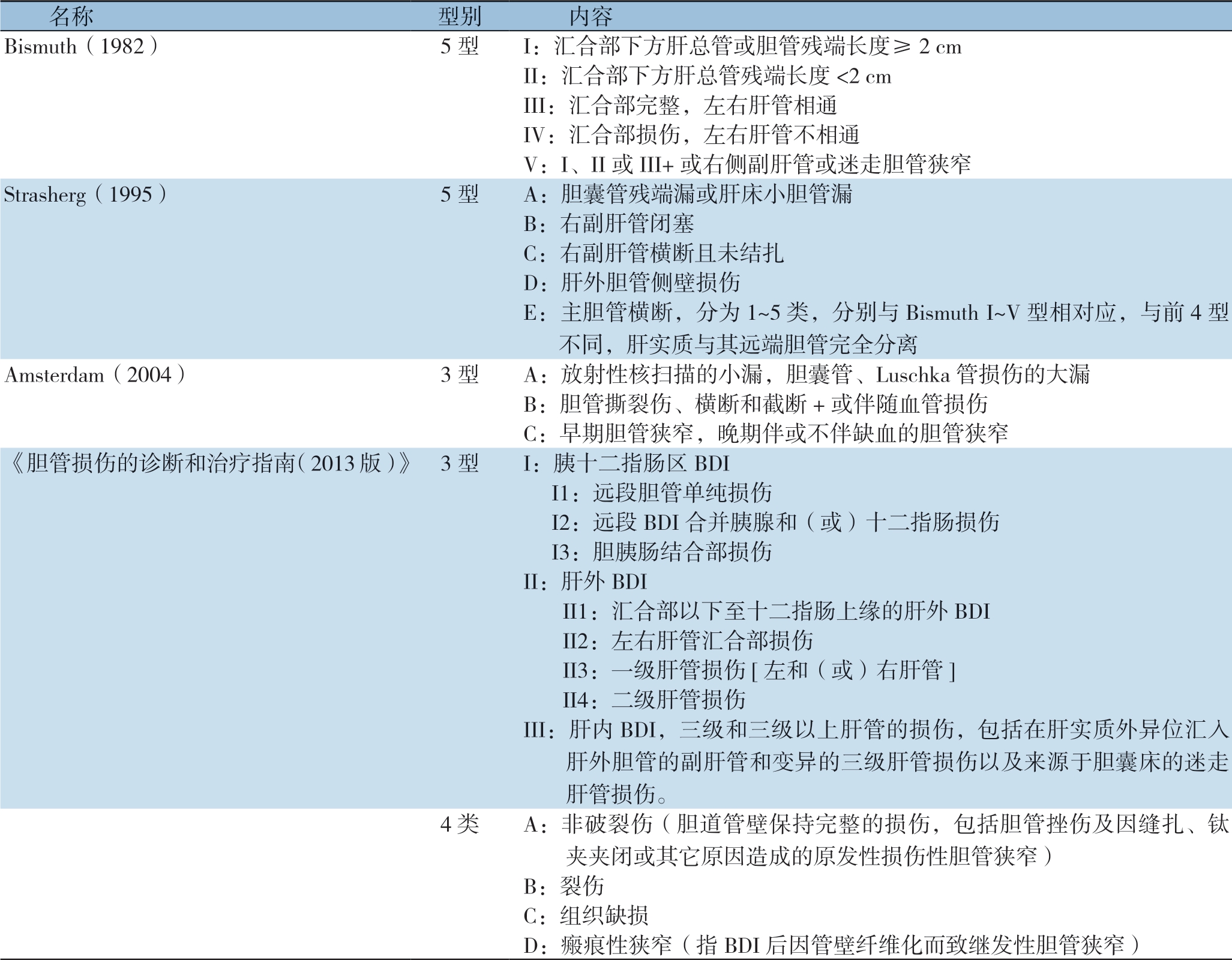
3 分 型
诊断BDI的分型很多,最被认可的是Bismuth分型[5],基于左右肝管汇合部距离(简称 汇合部)不包括BDI整个范围,常用于OC或其他手术(甚至非胆囊切除手术)。而同样被广为熟知的Strasherg分型[20]用于LC,是Bismuth补充,包括所有损伤类型及能被分类BDL。其他各种分型不断被提出,Amsterdam分型[21]是Bergman新修订分型,将BDI从小且无症状BDL扩大到截断整个分岔并损伤血管及治疗后并发症范围。我国2013版胆管损伤诊治指南[22],以胆管系统解剖为基础,涉及损伤的病理特征。各种分型具体内容见表1。
表1 LC 相关BDI 的主要分型
Table1 The main classifications of LC-associated BDI
名称 型别 内容Bismuth(1982) 5 型 I:汇合部下方肝总管或胆管残端长度≥2 cm II:汇合部下方肝总管残端长度<2 cm III:汇合部完整,左右肝管相通IV:汇合部损伤,左右肝管不相通V:I、II 或III+或右侧副肝管或迷走胆管狭窄Strasherg(1995) 5 型 A:胆囊管残端漏或肝床小胆管漏B:右副肝管闭塞C:右副肝管横断且未结扎D:肝外胆管侧壁损伤E:主胆管横断,分为1~5 类,分别与Bismuth I~V 型相对应,与前4 型不同,肝实质与其远端胆管完全分离Amsterdam(2004) 3 型 A:放射性核扫描的小漏,胆囊管、Luschka 管损伤的大漏B:胆管撕裂伤、横断和截断+或伴随血管损伤C:早期胆管狭窄,晚期伴或不伴缺血的胆管狭窄《胆管损伤的诊断和治疗指南(2013 版)》 3 型 I:胰十二指肠区BDI I1:远段胆管单纯损伤 I2:远段BDI 合并胰腺和(或)十二指肠损伤 I3:胆胰肠结合部损伤II:肝外BDI II1:汇合部以下至十二指肠上缘的肝外BDI II2:左右肝管汇合部损伤 II3:一级肝管损伤[左和(或)右肝管] II4:二级肝管损伤III:肝内BDI,三级和三级以上肝管的损伤,包括在肝实质外异位汇入肝外胆管的副肝管和变异的三级肝管损伤以及来源于胆囊床的迷走肝管损伤。4 类 A:非破裂伤(胆道管壁保持完整的损伤,包括胆管挫伤及因缝扎、钛夹夹闭或其它原因造成的原发性损伤性胆管狭窄)B:裂伤C:组织缺损D:瘢痕性狭窄(指BDI 后因管壁纤维化而致继发性胆管狭窄)
4 治 疗
4.1 经验培训
4.1.1 解剖 Strasberg 等[20]提出腔镜手术安全视图(critical view of safety,CVS)技术,Russell 等总结:⑴ 充分暴露Calot 三角;⑵ 将Hartmann 囊袋侧部及下部牵拉打开胆囊管和肝总管之间角度避免解剖误认;⑶ Calot 三角需尽可能除去脂肪并分离组织间隙;⑷ 从胆囊颈部(以淋巴结为标志)开始,由侧面向中间剥离,尽量保持胆囊完整;⑸ 合理使用低阈值电烧灼解剖胆管,避免出血和BDL[4]。
4.1.2 经验 LC 需专业术者和技术,BDI 难以避免,仅30% 在初次手术中被发现,若经验不足修复手术难以进行,其中75% 由首诊医生参与,而修复成功率只有17%[23]。
4.1.3 决策 BDI 被确诊,首先控制脓毒及持续性BDL,识别BDL 源头并控制进展是重点。若胆管延续性存在,支架帮助修复,手术重建常在控制感染后[24]。首诊医生提供如抗生素、感染程度、再入院时间及手术过程等信息,BDI 增加3 倍死亡风险,综合性诊疗中心具有丰富经验及承担治疗无效风险能力,所以转诊综合性医院以及首诊医生参与很重要[11]。
4.2 分期下不同辅助器械治疗
4.2.1 术中 IOC 识别胆管解剖及损伤程度。研究[25]称LC 中IOC 有效,是诊断BDI 金标准。
4.2.2 术后 ⑴ 小漏:第一,可经Vater 乳头用支架或鼻胆管引流,1~5 d 小BDL 闭合。由鼻胆管置入胆道镜镜检,虽无需移除导管、重复ERCP[17],但有不适感、管子移位、体液丢失、电解质失衡及增加住院时间等缺点。第二,伴胆管狭窄,需行括约肌切开,但对支架尺寸、数量、形态、长度及放置时间等存争议。另外,需再次手术取出支架,治愈率达66%~100%,失败应怀疑更严重BDI[24]。⑵ 大漏:大多经支架修复。胆管旁路BDL 若有交通性漏及难辨认异常胆管,可内镜引导支架引流以避免腹部脓肿形成,6~8 周后取出支架或T 管。若都失败,内镜下行N- 丁酰基-2- 氰基丙烯酸盐粘合剂阻塞瘘[26]。⑶ 胆管狭窄,首选ERCP,经扩张器置入支架。建议放置至少1年,每3~4 个月置换至少2 个3.3 mm 支架。若1年后治疗失败,再次狭窄疑伴有缺血[24]。
4.3 手术
4.3.1 手术方式 胆管重建条件是吻合口边缘健康,长度至少1.5 cm,在感染控制后行无张力吻合术[14]。常用方法有端端胆管吻合(end-toend ductal biliary anastomosis,EE)、Roux-en-Y[肝管/胆管空肠吻合(hepaticojejunostomy,HJ;choledochojejunostomy,CJ)]、 胆管十二指肠吻合(choledochoduodenostomy,CD)、肝脏切除(Liver resection,LR)、 肝移植(liver transplantation,LT)。
⑴ EE:更多用于LT患者,保留胃肠管胆汁流向生理结构,减少溃疡发生[27]。研究[11]称损伤胆管(汇合部<2 cm)即使达4 cm,EE联合T管行微型吻合[28-29]。但即便行Kocher手法即移动胰头十二指肠,仍有吻合口狭窄风险,Thethy等[30]报道称EE并放置支架再狭窄率比CD不放置支架还高。⑵ CD:很少使用,仅用于胆总管远端损伤。Tocchi等[31]分析1 003例经历不同胆肠吻合,55例(5.5%)术后发生胆管肿瘤,发生率是CD为7.6%,Roux-en-Y HJ为1.9%。CD虽保留生理结构,但引起胃肠道反流、胆管炎复发及胆管新生物形成,再狭窄发生率高于Roux-en-Y[21]。⑶ Roux-en-Y:应用最为广泛。Liu等[3 2]分析 3例,据Strasberg分型有E2、E4、E4,分别行放支架、仅缝合、部分I区尾状叶肝切,并行HJ,预后良好。Głuszek等[33]分析8例,分别为4例肝总管、2例胆总管、1例右肝管、1例Luschka管部位BDI,除1例Luschka管行ERCP行夹闭术,均行Roux-en-Y HJ;3例死亡,1例再发胆管炎反复住院,余预后可。胆管(其中胆总管常<7 mm)对吻合技术要求高、容易狭窄是其技术难点[30]。损伤达更高部位胆管或狭窄完全横断,因吻合口血供差且张力不可靠,将致BDL及继发胆管硬化(secondary biliary cirrhosis,SBC),建议再行Roux-en-Y。若吻合部位有狭窄及炎症限制,推荐垂直切口及水平切口缝合为重建2~3 cm宽吻合方法。⑷ LR:复杂BDI 时,可选择性使用。 Li等[34-35]分析近端BDI伴或不伴VI的LC后BDI患者早晚需行LR,区别在于损伤诱导肝坏死需要早起干预,而为治疗长期胆管炎引起的肝萎缩需切除。而Liu等[32]分析肝内二级及以上胆管狭窄、血管损伤或肝囊肿发生肝萎缩,需要LR。总之,近端胆管(侵及汇合部)复杂BDI伴行血管损伤(vascular injury,VI),导致肝坏死及长期胆管炎肝萎缩,则需部分LR。另外,一些复杂损伤为良好暴露正常胆管,如切除IV区肝方叶便于探查肝内胆管。⑸ LT:其他治疗方式无效,可选择性使用。Lubikowski等[36]分析2例,Strasberg分型为B和E3,均未伴行VI,经历胆管探查、胆管重建、HJ、T管引流等治疗,因SBC行LT,行LT中行胆管吻合、端侧胆管十二指肠吻合等胆道重建。随访中无死亡病例。Parrilla等[37]分析14例,Strasberg分型1 例E 2、3例E 3、10例E4,其中有7 例伴行VI,13例行手术,1例保守;7例急性肝衰竭,7例胆肠吻合引起SBC;行LT后,6例死亡。总之,严重BDI引起急慢性肝损伤,如伴行门静脉、肝动脉损伤或SBC导致横断胆管等,LT是肝衰患者最后选择[38]。
4.3.2 手术时机 需结合症状,损伤类型和专业经验等方面考虑[32]。多数LC 术后BDI 无症状,比较早期、中期(72 h 至6 周)及晚期修复,显示是否手术与血清胆红素的降低及炎症控制有关。紧急手术仍具争议,早期发现并无胆管漏、脓肿形成和脓毒表现,可立即重建。术中发现BDI 应求助有经验医师,是否行肝胆管重建。所以建议:⑴ 立即手术(术中发现BDI);⑵ 早期手术(近端胆管是完全被堵塞的,无BDL);⑶ 晚期手术(出现胆管炎,胆道脓毒)[13, 39-41]。
5 预 后
据McDonal等[42]胆管修复有效性:A类,无症状,正常肝功能;B类,无症状,肝功能轻度升高,周期性疼痛或发热;C类,疼痛,胆管炎伴有黄疸性发热和肝功能异常;D类,需手术或内镜。总之,A、B类预后良好,而C、D类预后不良。超声是随访中重要工具,BDL是唯一重要独立预测指标。短期随访示良好预后;中期随访(6~ 102个月,平均59个月)示HJ术后88%~92%良好肝功能,但增加BDL。HJ术后晚期吻合口狭窄发生率4%~24%;而长期随访(超5年)示手术重建成功率达84%,延迟重建94%成功率、无致死率[14, 43-44]。
6 总 结
胆囊切除术引起BDI研究仍有很多未解决问题:⑴ LC比OC具更高BDI发生率,虽然仍存疑甚至否认,但研究更支持LC引起更高BDI发生率,甚至有倍数关系。⑵ BDI临床表现各异,需从术中与术后分析,依靠症状、体征、检验检查、经验等判断。⑶ IOC使用存在争议,由于IOC技术具有一定特殊性,需要结合术前术中情况,尤其影像学的评估及经验的积累综合考虑,对其利弊性尚无明确结论。⑷ BDI分类不断被完善,各种分类更多追求全面性,谋求从诊断乃至治疗整体观念进行划分。⑸ 另外,McCormack等[45]报道,LC中血管和BDI导致缺血性肝坏死引发急性肝衰竭,术中肝门部出血及时行中转开腹,多处缝扎肝实质止血,损伤右肝动脉及右门静脉,肝坏疽的急性肝衰竭,严重凝血障碍和进行性继发多器官衰竭,行LT后,24 h后死亡。不难发现,BDI治疗方法的多样化,如内镜下支架、引流等保守治疗,但更多积极手术治疗,手术方式依靠狭窄部位及分型、阻塞程度、修复及时性、术者经验等综合选择[46]。在LC中识别BDI,可行IOC并中转开腹明确损伤范围,修复应由有经验的医生,不具条件应在放置引流转诊上级医院[27, 47]。不同治疗方案都会影响患者预后,但这些方法并不独立,而是具体问题具体分析,将方法整合后应用于实际[30]。随着LC使用越广泛,而LC引起BDI并发症更引起关注,而对BDI修复治疗的规范化也在积极的探讨中。
[1] Dubois F, Icard P, Berthelot G, et al. Coelioscopic cholecystectomy. Preliminary report of 36 cases[J]. Ann Surg, 1990, 211(1):60-62.
[2] Karvonen J, Salminen P, Gronroos JM. Bile duct injuries during open and laparoscopic cholecystectomy in the laparoscopic era: alarming trends[J]. Surg Endosc, 2011, 25(9):2906-2910. doi: 10.1007/s00464-011-1641-1.
[3] 蔡秀军. 腹腔镜在腹部外科应用的现状及发展方向[J]. 中华医学杂志, 2005, 85(3):145-148. doi:10.3760/j:issn:0376- 2491.2005.03.001. Cai XJ. Laparoscopic surgery in the treatment of abdominal diseases:present status and prspects[J]. National Medical Journal of China, 2005, 85(3):145-148. doi:10.3760/j:issn:0376-2491.2005.03.001.
[4] Beckingham IJ. Gallstones[J]. Surgery (Oxford), 2017, 35(12):682. doi: https://doi.org/10.1016/j.mpsur.2017.09.013.
[5] Sajid MS, Leaver C, Haider Z, et al. Routine on-table cholangiography during cholecystectomy: a systematic review[J]. Ann R Coll Surg Engl, 2012, 94(6):375-380. doi: 10.1308/0035884 12X13373405385331.
[6] Parmeggiani D, Cimmino G, Cerbone D, et al. Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review[J]. G Chir, 2010, 31(1/2):16-19.
[7] Koike D, Suka Y, Nagai M, et al. Laparoscopic Management of Mirizzi Syndrome Without Dissection of Calot's Triangle[J]. J Laparoendosc Adv Surg Tech A, 2017, 27(2):141-145. doi: 10.1089/lap.2016.0426.
[8] Jung HS, Huh K, Shin YH, et al. Left-sided gallbladder: a complicated percutaneous cholecystostomy and subsequent hepatic embolisation[J]. Br J Radiol, 2009, 82(979):e141-144. doi: 10.1259/bjr/59092209.
[9] 陈智勇, 陈文有, 杨爱国. 腹腔镜胆囊切除术并发症发生的相关影响因素分析[J]. 中国普通外科杂志, 2016, 25(2):214-218. doi:10.3978/j.issn.1005-6947.2016.02.010. Chen ZY, Chen WY, Yang AG. Analysis of influential factors for complications associated with laparoscopic cholecystectomy[J]. Chinese Journal of General Surgery, 2016, 25(2):214-218. doi:10.3978/j.issn.1005-6947.2016.02.010.
[10] Francoeur JR, Wiseman K, Buczkowski AK, et al. Surgeons' anonymous response after bile duct injury during cholecystectomy[J]. Am J Surg, 2003, 185(5):468-475.
[11] Bobkiewicz A, Krokowicz Ł, Banasiewicz T, et al. Iatrogenic bile duct injury. A significant surgical problem. Assessment of treatment outcomes in the department's own material[J]. Pol Przegl Chir, 2015, 86(12):576-583. doi: 10.1515/pjs-2015-0004.
[12] Sicklick JK, Camp MS, Lillemoe KD, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients[J]. Ann Surg, 2005, 241(5):786-792.
[13] Archer SB, Brown DW, Smith CD, et al. Bile duct injury during laparoscopic cholecystectomy: results of a national survey[J]. Ann Surg, 2001, 234(4):549-558.
[14] Hajjar NA, Tomuş C, Mocan L, et al. Management of bile duct injuries following laparoscopic cholecystectomy: long-term outcome and risk factors infuencing biliary reconstruction[J]. Chirurgia (Bucur), 2014, 109(4):493-499.
[15] Yi F, Jin WS, Xiang DB, et al. Complications of laparoscopic cholecystectomy and its prevention: a review and experience of 400 cases[J]. Hepatogastroenterology, 2012, 59(113):47-50. doi: 10.5754/hge11232.
[16] Aduna M, Larena JA, Martín D, et al.Bile duct leaks after laparoscopic cholecystectomy: value of contrast-enhanced MRCP[J]. Abdom Imaging, 2005, 30(4):480-487. doi: 10.1007/s00261-004-0276-2.
[17] 刘平西, 周钧, 唐腾龙, 等. 腹腔镜胆囊切除术联合ERCP解决术中棘手问题30例分析[J]. 中国普通外科杂志, 2015, 24(2):293-296. doi:10.3978/j.issn.1005-6947.2015.02.028. Liu PX, Zhou J, Tang TL, et al. The solution of difficult problems encountered during laparoscopic cholecystectomy combined with endoscopic retrograde cholangiopancreatography:an analysis of 30 cases[J]. Chinese Journal of General Surgery, 2015, 24(2):293-296. doi:10.3978/j.issn.1005-6947.2015.02.028.
[18] 陈章彬, 陈见中, 滕毅山. 经皮经肝穿刺胆道引流术在腹腔镜下胆道探查术后一期缝合中的应用价值[J]. 中国普通外科杂志, 2018, 27(2):156-162. doi:10.3978/j.issn.1005-6947.2018.02.004. Chen ZB, Chen JZ, Teng YS. Application value of percutaneous transhepatic cholangial drainage in laparoscopic common bile duct exploration with primary closure[J]. Chinese Journal of General Surgery, 2018, 27(2):156-162. doi:10.3978/j.issn.1005-6947.2018.02.004.
[19] Wojcicki M, Patkowski W, Chmurowicz T, et al. Isolated right posterior bile duct injury following cholecystectomy: report of two cases[J]. World J Gastroenterol, 2013, 19(36):6118-6121. doi: 10.3748/wjg.v19.i36.6118.
[20] Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy[J]. J Am Coll Surg, 1995, 180(1):101-125.
[21] Rauws EA, Gouma DJ. Endoscopic and surgical management of bile duct injury after laparoscopic cholecystectomy[J]. Best Pract Res Clin Gastroenterol, 2004, 18(5):829-846. doi: 10.1016/j.bpg.2004.05.003.
[22] 中华医学会外科学分会胆道外科学组. 胆管损伤的诊断和治疗指南(2013版)[J]. 中华消化外科杂志, 2013, 12(2):81-95. doi:10.3760/cma.j.issn.1673-9752.2013.02.001. Biliary Surgery Group of Surgery Branch of Chinese Medical. Association. Practice guideline for diagnosis and treatment of bile duct injury(2013 edition) [J]. Chinese Journal of Digestive Surgery, 2013, 12(2):81-95. doi:10.3760/cma.j.issn.1673-9752.2013.02.001.
[23] Massarweh NN, Devlin A, Symons RG, et al. Risk tolerance and bile duct injury: surgeon characteristics, risk-taking preference, and common bile duct injuries[J]. J Am Coll Surg, 2009, 209(1):17-24. doi: 10.1016/j.jamcollsurg.2009.02.063.
[24] Chinnery GE, Krige JE, Bornman PC, et al. Endoscopic management of bile leaks after laparoscopic cholecystectomy[J]. S Afr J Surg, 2013, 51(4):116-121. doi: 10.7196/sajs.1829.
[25] Buddingh KT, Weersma RK, Savenije RA, et al. Lower rate of major bile duct injury and increased intraoperative management of common bile duct stones after implementation of routine intraoperative cholangiography[J]. J Am Coll Surg, 2011, 213(2):267-274. doi: 10.1016/j.jamcollsurg.2011.03.004.
[26] Beliaev AM, Booth M. Late two-stage laparoscopic cholecystectomy is associated with an increased risk of major bile duct injury[J]. ANZ J Surg, 2016, 86(1/2):63-68. doi: 10.1111/ans.12967.
[27] Jabłońska B, Lampe P, Olakowski M, et al. Hepaticojejunostomy vs. end-to-end biliary reconstructions in the treatment of iatrogenic bile duct injuries[J]. J Gastrointest Surg, 2009, 13(6):1084-1093. doi: 10.1007/s11605-009-0841-7.
[28] Jablonska B. End-to-end ductal anastomosis in biliary reconstruction: indications and limitations[J]. Can J Surg, 2014, 57(4):271-277.
[29] 兰军良, 董晓勇, 畅文玲, 等. 腹腔镜胆囊切除术胆管损伤的诊治分析[J]. 中国普通外科杂志, 2017, 26(8):1076-1080. doi:10.3978/j.issn.1005-6947.2017.08.018. Lan JL, Dong XY, Chang WL, et al. Analysis of diagnosis and treatment of laparoscopic cholecystectomy- related bile duct injury[J]. Chinese Journal of General Surgery, 2017, 26(8):1076-1080. doi:10.3978/j.issn.1005-6947.2017.08.018.
[30] Thethy S, Thomson B, Pleass H, et al. Management of biliary tract complications after orthotopic liver transplantation[J]. Clin Transplant, 2004, 18(6):647-653. doi: 10.1111/j.1399-0012.2004.00254.x.
[31] Tocchi A, Mazzoni G, Liotta G, et al. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1,000 patients[J]. Ann Surg, 2001, 234(2):210-214.
[32] Liu H, Shen S, Wang YQ, et al. Biliary reconstruction and Rouxen-Y hepaticojejunostomy for the management of complicated biliary strictures after bile duct injury[J]. Int Surg J, 2015, 2(2):179-186.
[33] Gluszek S, Kot M, Balchanowski N, et al. Iatrogenic bile duct injuries--clinical problems[J]. Pol Przegl Chir, 2014, 86(1):17-25. doi: 10.2478/pjs-2014-0004.
[34] Li J, Frilling A, Nadalin S, et al. Timing and risk factors of hepatectomy in the management of complications following laparoscopic cholecystectomy[J]. J Gastrointest Surg, 2012, 16(4):815-820. doi: 10.1007/s11605-011-1769-2.
[35] Jablonska B. Hepatectomy for bile duct injuries: when is it necessary?[J]. World J Gastroenterol, 2013, 19(38):6348-6352. doi: 10.3748/wjg.v19.i38.6348.
[36] Lubikowski J, Chmurowicz T, Post M, et al. Liver transplantation as an ultimate step in the management of iatrogenic bile duct injury complicated by secondary biliary cirrhosis[J]. Ann Transplant, 2012, 17(2):38-44.
[37] Parrilla P, Robles R, Varo E, et al. Liver transplantation for bile duct injury after open and laparoscopic cholecystectomy[J]. Br J Surg, 2014, 101(2):63-68. doi: 10.1002/bjs.9349.
[38] de Santibañes E, Ardiles V, Gadano A, et al. Liver transplantation: the last measure in the treatment of bile duct injuries[J]. World J Surg, 2008, 32(8):1714-1721. doi: 10.1007/s00268-008-9650-5.
[39] Sahajpal AK, Chow SC, Dixon E, et al. Bile duct injuries associated with laparoscopic cholecystectomy: timing of repair and longterm outcomes[J]. Arch Surg, 2010, 145(8):757-763. doi: 10.1001/archsurg.2010.153.
[40] Zhou LK, Prasoon P. Mechanical and preventable factors of bile duct injuries during laparoscopic cholecystectomy[J]. Hepatogastroenterology, 2012, 59(113):51-53. doi: 10.5754/hge10249.
[41] 殷俊杰, 蔡阳, 张筱凤, 等. 腹腔镜胆囊切除术并发胆管损伤患者的诊治[J]. 中华肝胆外科杂志, 2016, 22(1):27-29. doi:10.3760/cma.j.issn.1007-8118.2016.01.008. Yin JJ, Cai Y, Zhang XF, et al. Diagnosis and treatment of patients with bile duct injury after laparoscopic cholecystectomy[J]. Chinese Journal of Hepatobiliary Surgery, 2016, 22(1):27-29. doi:10.3760/cma.j.issn.1007-8118.2016.01.008.
[42] McDonald ML, Farnell MB, Nagorney DM, et al. Benign biliary strictures: repair and outcome with a contemporary approach[J]. Surgery, 1995, 118(4):582-590.
[43] Lubikowski J, Post M, Bialek A, et al. Surgical management and outcome of bile duct injuries following cholecystectomy: a singlecenter experience[J]. Langenbecks Arch Surg, 2011, 396(5):699-707. doi: 10.1007/s00423-011-0745-3.
[44] Flum DR, Cheadle A, Prela C, et al. Bile duct injury during cholecystectomy and survival in medicare beneficiaries[J]. JAMA, 2003, 290(16):2168-2173. doi: 10.1001/jama.290.16.2168.
[45] McCormack L, Quiñonez EG, Capitanich P, et al. Acute liver failure due to concomitant arterial, portal and biliary injury during laparoscopic cholecystectomy: is transplantation a valid life-saving strategy? A case report[J]. Patient Saf Surg, 2009, 3(1):22. doi: 10.1186/1754-9493-3-22.
[46] Hall JG, Pappas TN. Current management of biliary strictures[J]. J Gastrointest Surg, 2004, 8(8):1098-1110. doi: 10.1016/j.gassur.2004.04.011.
[47] Jabłońska B, Lampe P. Iatrogenic bile duct injuries: etiology, diagnosis and management[J]. World J Gastroenterol, 2009, 15(33):4097-4104.
