颅内椎动脉夹层动脉瘤(vertebral artery dissecting aneurysm,VADA)发病率低(0.001%~0.0015%)[1],破裂的椎动脉夹层动脉瘤(ruptured vertebral artery dissecting aneurysm,RVADA)破裂出血及再发出血,病情凶险,病死率及致残率均高,有报道[2]保守治疗46.7%的患者再出血1周内死亡。由于介入治疗普及、及时、有效,已经成为该疾病的有效治疗方式,介入治疗多采用载瘤动脉闭塞的方法,不过依然有脑干、小脑梗塞的风险,而另外一种治疗方式保留载瘤动脉支架辅助栓塞VADA正越来越多的被大家采用,然而依然有许多不足,本研究报告28例治疗结果。
1 资料与方法
1.1 一般资料
入组标准:DSA造影下,有明确VADA异常影像者。如果是RVADA,CT提示自发性蛛网膜下腔出血或腰穿证实有蛛网膜下腔出血,结合影像学结果考虑椎动脉夹层动脉瘤为责任病灶者,排除外伤性者。自2013年1月—2018年10月,我中心采用支架辅助栓塞治疗VADA患者28例,其中男8例,女20例;年龄(51.8±7.5)岁。未破裂12例,临床表现未破裂者表现为头痛头晕;RVADA 16例为突发头痛,伴有恶心、呕吐,伴或不伴有意识障碍。破裂者格拉斯哥昏迷评分法(Glasgow Coma Scale,GCS)≥9分13例,GCS≤8分3例。Hunt-Hess分级I~III级以下12例,Hun-Hess分级IV~V级4例。
1.2 影像学资料
脑血管造影进行双侧椎动脉是否是优势供血、颈内动脉系统和椎基底动脉供血系统代偿评估,DSA显示受累有椎动脉扩张和狭窄或局部囊状扩张,重点分析受累节段是否累及小脑后下动脉(posterior inferior cerebellar artery,PICA)起始部,受累病变段是否有重要穿支支配脊髓前或脑干周围区域。未破裂动脉瘤手术前后行磁共振检查了解有无新发脑梗塞情况。破裂者术后行磁共振检查了解颅内病变情况。动脉瘤治疗术后即刻造影影像及随访影像采用Raymond分级[3]。
1.3 治疗方法
所有治疗均在全身麻醉下进行,术中使用肝素80 U/kg肝素化,自麻醉成功后开始,并每小时后半量追加肝素,直到用量为1 000 U维持,术中保持动脉通道滴注通畅。经股动脉入路置入6 F动脉鞘,经鞘置入6 F或者5 F Envoy导引导管(美国Johnson公司)至椎动脉平第二颈椎水平。治疗采用2枚或2枚以上Enterprise支架(美国Codman公司),支架输送导管为Headway 21(美国Microvention公司)或Prowler Select plus微导管(Prowler Select Plus,美国Codman公司),动脉瘤填塞微导管为Enchelon 10(Echlon-10,美国EV3公司)。支架的释放方式为首枚支架采用半释放,待动脉瘤囊状突起被满意填塞后再逐步完全释放支架,力求动脉瘤不显影,如果是多支架采用重叠释放方式。支架的长度选择应覆盖整个受累病变段。
未破裂VADA 12例,治疗前均使用波立维75 mg、阿司匹林100 mg口服3~5 d。RVADA患者16例均为急诊入院病例,并接受急诊手术,造影结束明确诊断后,治疗开始前给予波立维、阿司匹林各300 mg纳肛或经胃管注入,考虑到抗血小板聚集不充分,备用替罗非班(5 mg/100 mL),发现支架内血栓形成影像及前向血流变慢,根据体质量给予低剂量4~5 mL经动脉导管内灌注10 min,可重复使用至血栓消失或血流明显改善,同时用替罗非班(5 mg/100 mL)4 mL/h静脉泵入维持,共6 h(5 mg/100 mL)。破裂出血患者1例术前出现呼吸暂停,血氧下降,给予气管插管人工支持呼吸,并行脑室外引流手术,另外1例术后再行脑室外引流手术。其它治疗包括腰穿、使用预防脑血管痉挛、补液及营养支持、脱水及控制颅内压及对症处理等。
1.4 随访
患者术后3~6个月,12~18个月,24~36个月接受DSA脑血管造影随访或CTA、MRA复查。患者影像学随访采用改良Rankin量表(modified Rankin Scale,mRS)评分,预后不良者mRS≥3分[4]。
2 结 果
2.1 总体治疗情况
28例患者中支架辅助栓塞治疗技术成功率100%,未破裂者其中5例采用单纯2枚及2枚以上支架植入,术后即刻动脉瘤内造影剂滞留,随访发现动脉瘤消失或动脉瘤明显变小,Raymond分级I级3例,II级2例(图1),另23例采用支架辅助弹簧圈栓塞,术后即刻动脉瘤完全不显影Raymond分级I级11例(11/23),Raymond分级II级5例(5/23),Raymond分级III级7例(7/23),其中19例(19/23)获得DSA影像学成功随访,平均随访(14.5±7.9)个月 ,随访发现动脉瘤完全不显影Raymond分级I级16例(16/19),Raymond分级II级3例(3/19),无Raymond分级III级病例。随访中1例因其它原因死亡,3例无随访结果。

图1 单纯多支架植入
Figure 1 Simple multiple stent placement display of the aneurysm after stent placement;up
A:术前显示局部椎动脉狭窄伴扩张;B:支架植入后瘤体显影减少;C:Dyn CT显示双支架;D:随访血管重塑好
A: Preoperative angiography showing stenosis with dilation of the vertebral artery; B: Reduced C: Dyn CT showing the double stent; D: Good vascular remodeling during follow-
2.2 支架内血栓事件发生情况
12例未破裂VADA,术中术后未发生支架内血栓事件。16例RVADA,1例发生治疗中支架内血栓形成,经替罗非班动脉内联合静脉维持给药后,血栓消退,另外1例术后18 h发生意识恶化,给予替罗非班溶栓后,同时复查DSA造影,提示椎动脉穿支事件,重复小剂量替罗非班给药后穿支再次显影,患者病情迅速好转神志转清(图2)。
2.3 动脉瘤周邻血管分布情况
28例接受治疗的患者中,21例(21/28)影像学上表现为病变段明显囊状膨出,5例(5/28)累及小脑下后动脉(图3),4例(4/28)有明显细穿支血管发出,2例(2/28)病变血管对侧发育不良,代偿供血缺乏。16例(16/28)表现为明显的病变侧血管向基底动脉主要供血。
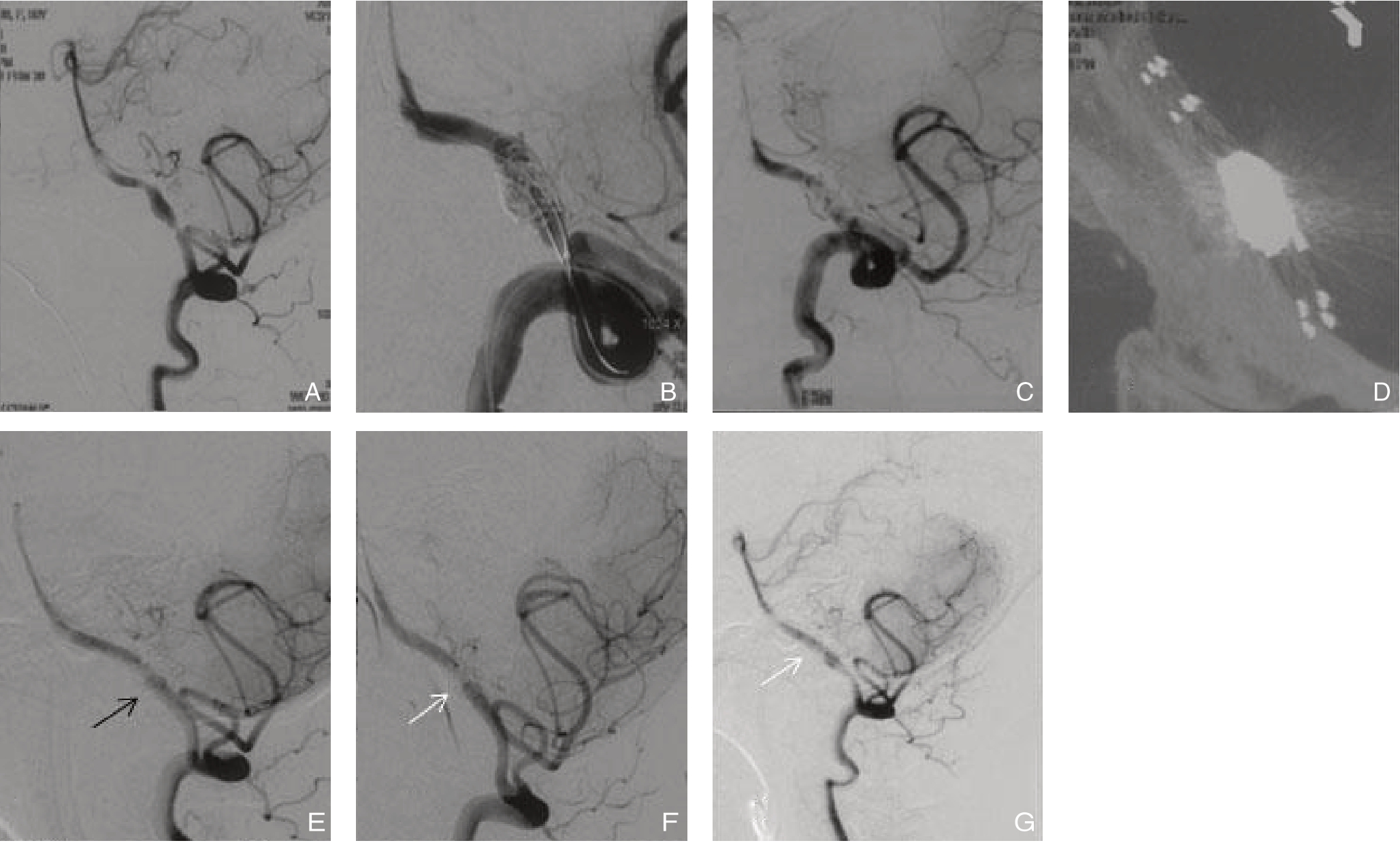
图2 多支架辅助弹簧圈栓塞
Figure 2 Multiple stent assisted coil embolization
A:病变受累位置有穿支发出;B:半释放技术填塞动脉瘤,保护穿支;C:双支架辅助弹簧圈栓塞后,动脉瘤不显影,穿支显影,血管较术前变直;D:Dyn CT显示双支架辅助弹簧圈;E:术后18 h出现意识障碍,DSA复查见穿支不显影(黑箭头);F:术中溶栓患者意识恢复,穿支再次显示(白箭头);G:复查血管重塑良好穿支存在(白箭头)
A: Perforating branches coming off around the affected site; B: Tamping the aneurysm with semi-release technique for protection of the perforating branches; C: No display of the aneurysm, and display of the perforating branches with the vessel becoming more straight after double stent assisted coil embolization; D: Dyn CT showing the double stent assisted coil; E: Disturbance of consciousness 18 h after operation, and DSA showing no display of the perforating branches (black arrow); F: Consciousness recovery after thrombolysis and the perforating branches presented again (white arrow); G: Good vascular remodeling and presence of the perforating branches (white arrow)
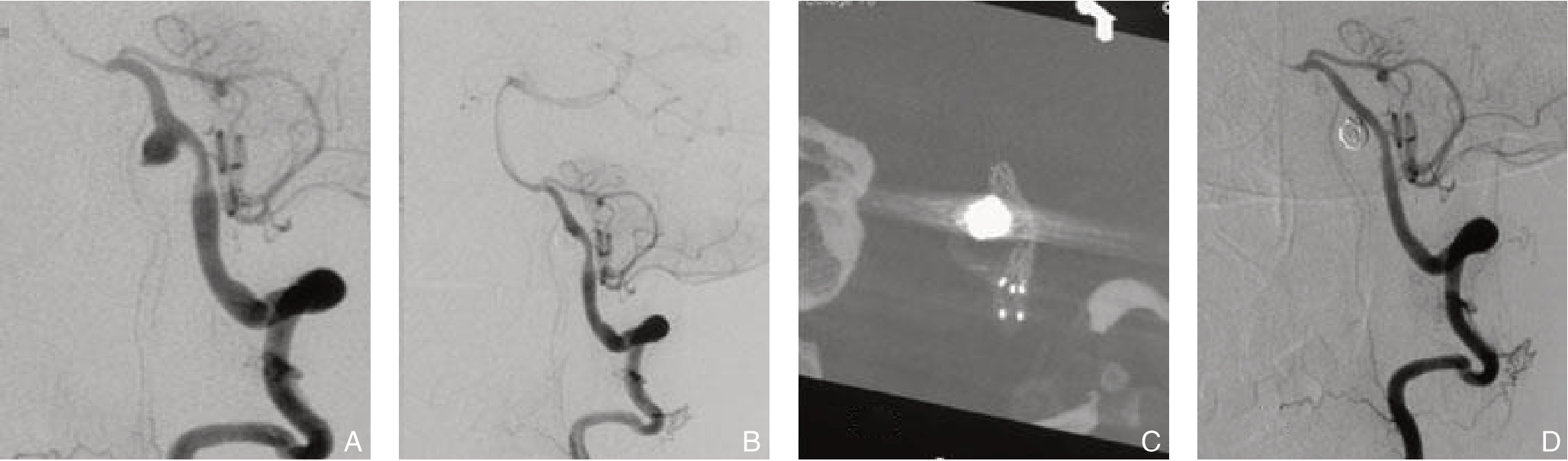
图3 病变累及小脑下后动脉的处理
Figure 3 Treatment of the lesion involving the posterior inferior cerebellar artery
A:破裂动脉瘤累及小脑下后动脉;B:双支架辅助弹簧圈栓塞动脉瘤凸起薄弱部分;C:Dyn CT显示双支架辅助弹簧圈栓塞;D:随访结果动脉瘤隔绝于血流外,血管重塑,血管较术前变直
A: The ruptured aneurysm involving the posterior inferior cerebellar artery; B: Double stent assisted coil embolization of the weak portion of the aneurysm; C: Dyn CT showing the double stent assisted coil; D: Follow-up result showing the aneurysm excluded from blood flow, vascular remodeling and straightened vessel
2.4 预后情况
随访期间,27例(27/28)mRS≤2分;不良预后mRS≥3分者1例(1/28),为入院时Hunt-Hess分级IV患者。
3 讨 论
自发性VADA发病率低,但其破裂瘤病情凶险,再发出血发生率高,病死率高,防止其再发出血是治疗关键[5]。载瘤动脉闭塞是常用的方法,但该方法在治疗动脉瘤的同时以牺牲载瘤动脉为代价,缺点也是治疗中必须关注的内容[6-7]。导致延髓、脊髓、小脑的梗死等,并且闭塞后再通也会发生,再次引起动脉瘤破裂[8-9]。消除动脉瘤同时保留载瘤动脉理论上最为合理,但需要对异常结构的血管进行重建,其中的方法各不相同,结果也各异[10-13]。 笔者采用单纯多重Enterprise支架或支架辅助弹簧圈栓塞的方法治疗VADA,单纯多重支架全部应用于其中5例未破裂动脉瘤患者,随访发现动脉瘤消失或缩小,结果令人满意。另外23例患者有明显动脉瘤瘤腔的椎动脉夹层动脉瘤,采用支架辅助弹簧圈栓塞的方法 ,临床结果能够有效的防止再出血,尽管术后即刻影像学结果动脉瘤还不能完全闭塞,但成功影像学随访19例结果发现动脉瘤完全不显影增加或残留明显减少,无Raymond分级III级病例出现。
采用保留载瘤动脉方式治疗VADA的常见原因:⑴ 椎动脉独立供血基底动脉,或病变侧椎动脉为主要供血对侧椎动脉发育不良,或代偿供血不充分;⑵ 动脉瘤累及PICA;⑶ 动脉瘤累及重要穿支如脑干周围穿支或脊髓前动脉[14];⑷ 夹层动脉瘤形态向侧方膨出适合保留载瘤动脉。由于一侧载瘤动脉闭塞,有增加另外一侧椎动脉形成动脉瘤的潜在风险[15],笔者采取尽量保留载瘤动脉的方式,对技术上能采用支架辅助弹簧圈的病例尽量采用该方式治疗。理由:⑴ 防止再出血是破裂椎动脉夹层动脉瘤治疗的主要目标之一[16],动脉瘤的出血一般不是持续的出血,持续出血的病例很难有获得治疗的机会,形态学上凸起最明显的地方通常被认为是破裂处,如果优先对破裂点填塞促使血栓形成,动脉瘤可以得到一定的保护[17];⑵ VADA并不是整个血管全周损坏,支架治疗除了其保护弹簧圈突入载瘤动脉、支架植入后“脚手架”作用、炎症作用外,还可以借助于多支架的血流导向作用[18],促进血管薄弱部分内弹簧圈治疗后血栓形成与修复;⑶ 由于椎动脉位于蛛网膜下腔使用Enterprise支架相对于其他编织型支架,更有利于病变段血管拉直,减少血流对动脉瘤体的冲击,这也是本组病例均采用Enterprise支架的理由之一。急性破裂期使用血流导向装置依然有争议[19-20],是否使用Enterprise联合血流导向支架治疗更加合理还需要更多病例的总结[20]。
血管内支架使用通常采用阿司匹林联合波立维抗血小板聚集,急性破裂期给与负荷量各300 mg,由于较多患者从影像学确诊RVADA到介入治疗结束不到3 h,抗血小板聚集不充分容易导致支架内血栓或栓塞事件[21],笔者在未破裂VADA患者中未发现有血栓事件发生,在破裂病例给予负荷量患者中出现支架内血栓和术后穿支事件,给予低剂量的替罗非班,维持6 h,获得满意的临床结果,由于病例数少,仍需要积累观察。
保持载瘤动脉通畅,不轻易牺牲血管具有重要意义,可以获得较好的临床结果,即使影像学上残留或复发,预后也可能较载瘤动脉闭塞后动脉瘤复发再通预后好[22],该方法是否作为VADA治疗的首选值得进一步观察。
[1]Schievink WI. Spontaneous dissection of the carotid and vertebral arteries[J]. N Engl J Med, 2001, 344(12):898-906. doi: 10.1056/NEJM200103223441206.
[2]Mizutani T, Aruga T, Kirino T, et al. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms[J]. Neurosurgery, 1995, 36(5):905-912.doi: 10.1227/00006123-199505000-00003.
[3]袁金龙, 方兴根, 赵心同, 等. 多支架辅助弹簧圈治疗颈内动脉血泡样动脉瘤的疗效分析[J]. 医学研究生学报, 2018, 31(3):258-261. doi:10.16571/j.cnki.1008-8199.2018.03.008.Yuan JL, Fang XG, Zhao XT, et al. Overlapping stent-assisted coiling for blood blister-like aneurysms of the internal carotid artery[J]. Journal of Medical Postgraduates, 2018, 31(3):258-261. doi:10.16571/j.cnki.1008-8199.2018.03.008.
[4]王梦宇, 王兵, 吴斐, 等. 复合手术治疗慢性症状性颈内动脉闭塞[J]. 中国普通外科杂志, 2018, 27(12):1614-1619. doi:10.7659/j.issn.1005-6947.2018.12.019.Wang MY, Wang B, Wu F, et al. Combined operative treatment for chronic symptomatic carotid artery occlusion[J]. Chinese Journal of General Surgery, 2018, 27(12):1614-1619. doi:10.7659/j.issn.1005-6947.2018.12.019.
[5]Lee M, Park IS, Lee KH, et al. Endovascular Treatments for Ruptured Intracranial Vertebral Artery Dissecting Aneurysms: Experience in 16 Patients[J]. J Cerebrovasc Endovasc Neurosurg, 2017, 19(4):268-275.doi: 10.7461/jcen.2017.19.4.268.
[6]Aihara M, Naito I, Shimizu T, et al. Predictive factors of medullary infarction after endovascular internal trapping using coils for vertebral artery dissecting aneurysms[J]. J Neurosurg, 2018, 129(1):107-113.doi: 10.3171/2017.2.JNS162916.
[7]Kanematsu Y, Satomi J, Korai M, et al. Flow alteration therapy for ruptured vertebral artery dissecting aneurysms involving the posterior inferior cerebellar artery[J]. Neurol Med Chir (Tokyo), 2018, 58(8):341-349.doi:10.2176/nmc.oa.2018-0076.
[8]Tanabe J, Moroi J, Yoshioka S, et al. Recanalization of a ruptured vertebral artery dissecting aneurysm after occlusion of the dilated segment only[J]. Surg Neurol Int, 2014, (5):150. doi:10.4103/2152-7806.143362.
[9]Ihn YK, Sung JH, Byun JH. Antegrade recanalization of parent artery after internal trapping of ruptured vertebral artery dissecting aneurysm[J]. J Korean Neurosurg Soc, 2012, 51(5):301-304. doi:10.3340/jkns.2012.51.5.301.
[10]Lim SH, Shin HS, Lee SH, et al. Endovascular treatment of vertebral artery dissecting aneurysms that cause subarachnoid hemorrhage : Consideration of therapeutic approaches relevant to the angioarchitecture[J]. J Korean Neurosurg Soc, 2015, 58(3):175-183. doi: 10.3340/jkns.2015.58.3.175.
[11]宣家龙, 雍成明, 杨代明, 等. 3D-CTA在破裂动脉瘤诊断及指导治疗中的价值[J]. 中国普通外科杂志, 2018, 27(12):1609-1613. doi:10.7659/j.issn.1005-6947.2018.12.018.Xuan JL, Yong CM, Yang DM, et al. Value of 3D-DSA and 3D-CTA in diagnosis and therapeutic guidance for rupture of arterial aneurysm[J]. Chinese Journal of General Surgery, 2018, 27(12):1609-1613. doi: 10.7659/j.issn.1005-6947.2018.12.018.
[12]邢晓锋, 施铭岗, 佟小光. 血流重建方法治疗复杂小脑后下动脉近端动脉瘤[J]. 中华神经外科杂志, 2019, 35(3):293-297. doi:10.3760/cma.j.issn.1001-2346.2019.03.013.Xing XF, Shi MG, Tong XG. Revascularization treatment for complex proximal posterior inferior cerebellar artery aneurysms[J]. Chinese Journal of Neurosurgery, 2019, 35(3):293-297. doi:10.3760/cma.j.issn.1001-2346.2019.03.013.
[13]Akamatsu Y, Sato K, Endo H,et al.Ruptured Vertebral Artery Dissecting Aneurysm Concurrent with Spontaneous Cervical Internal Carotid Artery Dissection: A Report of Three Cases and Literature Review[J]. World Neurosurg, 2017, 107:1048.e1-1048.e6. doi:10.1016/j.wneu.2017.08.016.
[14]Tomura N, Kono K, Okada H, et al. A Ruptured Vertebral Artery Dissecting Aneurysm Involving the Anterior Spinal Artery:A Case Report[J]. No Shinkei Geka, 2016, 44(7):575-581. doi:10.11477/mf.1436203333.
[15]Kidani N, Sugiu K, Hishikawa T, et al. De novo vertebral artery dissecting aneurysm after internal trapping of the contralateral vertebral artery[J]. Acta Neurochir (Wien), 2017, 159(7):1329-1333. doi:10.1007/s00701-017-3204-2.
[16]王奉淼, 王静凛, 张海兵, 等. 双LVIS支架重叠辅助弹簧圈栓塞破裂椎动脉夹层动脉瘤[J]. 医学与哲学, 2018, 39(4):40-42. doi:10.12014/j.issn.1002-0772.2018.02b.11.Wang FM, Wang JL, Zhang HB, et al. Double LVIS Stent Overlapping Assisted Coil Embolization Ruptured Vertebral Artery Dissecting Aneurysm[J]. Medicine & Philosophy, 2018, 39(4):40-42. doi:10.12014/j.issn.1002-0772.2018.02b.11.
[17]程建杰, 张昌伟, 何吉福, 等. LVIS支架辅助弹簧圈治疗颈内血泡样动脉瘤[J]. 中国介入影像与治疗学, 2019, 16(4):253-255. doi:10.13929/j.1672-8475.201811009.Cheng JJ, Zhang CW, He JF, et al. LVIS stent assisted coil in treatment of internal carotid artery blood blister-like aneurysms [J]. Chinese Journal of Interventional Imaging and Therapy, 2019, 16(4):253-255. doi:10.13929/j.1672-8475.201811009.
[18]Li W, Liu J, Zhang Y, et al. Flow diversion and outcomes of vertebral fusiform aneurysms after stent-only treatment: A hemodynamic study[J]. World Neurosurg, 2017, 107:202-210. doi:10.1016/j.wneu.2017.07.157.
[19]Fang YB, Wen WL, Yang PF, et al. Long-Term Outcome of Tubridge Flow Diverter(S) in Treating Large Vertebral Artery Dissecting Aneurysms-A Pilot Study[J]. Clin Neuroradiol, 2017, 27(3):345-350. doi:10.1007/s00062-015-0494-8.
[20]Lim YC, Shin YS, Chung J. Flow Diversion via LVIS Blue Stent within Enterprise Stent in Patients with Vertebral Artery Dissecting Aneurysm[J]. World Neurosurg, 2018, 117:203-207. doi:10.1016/j.wneu.2018.06.029.
[21]谷鹏, 彭晨, 王伟, 等. 自发性孤立性肠系膜上动脉夹层的诊治:附3例报告[J]. 中国普通外科杂志, 2014, 23(6):780-784. doi:10.7659/j.issn.1005-6947.2014.06.015.Gu P, Peng C, Wang W, et al. Diagnosis and treatment of spontaneous isolated superior mesenteric artery dissection: a report of 3 cases[J]. Chinese Journal of General Surgery, 2014, 23(6):780-784. doi:10.7659/j.issn.1005-6947.2014.06.015.
[22]Sugiu K, Tokunaga K, Ono S, et al. Rebleeding from a vertebral artery dissecting aneurysm after endovascular internal trapping: adverse effect of intrathecal urokinase injection or incomplete occlusion?-case report-[J]. Neurol Med Chir (Tokyo), 2009, 49(12):597-600. doi:10.2176/nmc.49.597.
