深静脉血栓形成(deep venous thrombosis,DVT)是由于静脉血液异常凝集而引起的血液回流障碍,是住院患者常见的并发症,可表现为疼痛、肿胀、浅静脉曲张等[1]。19世纪中期,Virchow提出静脉血栓形成的三大因素,即静脉血流滞缓、静脉壁损伤和血液高凝状态[2]。ABO血型系统的抗原(A、B和H)由置于红细胞膜外表面的复杂碳水化合物分子组成,在我国ABO血型的表型分布频率随地区而变化,从北向西南的方向,O基因频率逐渐升高,频率分布大致为O型血35%,A型血28%,B型血29%,AB型血8%[3]。人类血型作为一个遗传标记与多种疾病有关[4]。Jick等[5]早在1969年发现非O型血型人群似乎更容易产生DVT。随后Gándara等[6-7]通过研究得到了相同的结果。但是,在2002年的一项创伤后DVT患者的回顾性研究中发现创伤患者DVT的发生与ABO血型之间没有关系[8],得出了与前述学者相反的结果。目前对于ABO血型与DVT的关系仍有争议。本文在统计苏北人民医院的DVT病例基础上,通过检索PubMed、CNKI、SionMed、万方、维普等数据库筛取相关文献,进行ABO血型系统与DVT发生风险的病例-对照研究及相关Meta分析,以期更好地明确ABO血型与DVT发生可能存在的关联,为DVT的个体化预防及精准治疗提供依据。
1 资料与方法
1.1 病例-对照研究
对苏北人民医院2012年10月—2018年12月的500例住院DVT患者(多次住院患者只统计首次住院)进行统计,按诱因分为无明显诱因组、妊娠组、外伤组、手术组、癌症组、长期卧床组。其中无明显诱因组267例(排除其他诱因,无阳性诊断),妊娠组3例(产褥期),外伤组73例(四肢及多发骨折患者),手术患者74例(排除骨折手术患者),癌症患者72例,长期卧床患者11例(因脑梗、昏迷及脊柱损伤卧床,平均卧床时间为(64.45±67.32)d,明确其年龄及血型分布。对照组按诱因1:1配对选取该院500例非DVT住院患者。对病例组和对照组进行统计学分析,计算不同诱因下患者的年龄(独立样本t检验)及血型(RR值及95% CI)与DVT发生的危险程度。
1.2 文献系统评价
1.2.1 检索策略与文献提取 检索PubMed、CNKI、SionMed、万方、维普数据库,文献语种不限,起始时间不限,截止时间为2019年10月1日,英文检索词包括:ABO Blood Group System;ABO Blood Group Systems;ABO Blood Group、H Blood Group System;H Blood Group;Blood Groups;H Blood Groups;ABH Blood Group;ABH Blood Groups;Blood Group H Type1 Antigen;ABO Factors;ABO Factor;Venous Thrombosis;Phlebothrombosis;Phlebothromboses;Venous Thrombose;Deep Vein Thrombosis;Deep Vein Thromboses 等。中文检索词包括:ABO 血型系统;静脉血栓形成等。手工检索正在进行的病例- 对照研究、专题报告、未发表的资料、会议文献等。由2 名研究人员独自阅读文题及摘要筛选相关文献,通过阅读全文对相关文献的研究设计、纳入排除标准、对照情况及研究结果判断方式进行评估,根据纳入排除标准选择是否将文件纳入Meta 分析。如存在争议,交由第3 名研究人员重新评估,并决定是否纳入分析。
1.2.2 文献纳入排除标准 纳入标准:(1)研究类型为病例- 对照研究;(2)文中病例组及对照组相关数据,均应由作者亲自调查所得;(3)对照组与病例组具有可比性(如选取同一医院同期的非DVT 患者作为对照);(4)诊断标准明确,病例组DVT 患者符合诊断标准;(5)基于同一样本的文献,只选取其中最详细数据报告的文献。排除标准:(1)文摘、综述等二、三次文献;(2)病例组、对照组样本的选取由他人文献加工而来;(3)对照组与病例组无可比性(如选择的人口样本不处于同一时期、存在区域差异,或选取特殊人群造成混杂影响);(4)无明确诊断标准,病例组未明确诊断证实;(5)无法获取详细资料的文献。
1.2.3 文献质量评价 由2 名研究人员独立采用纽卡斯尔- 渥太华量表(the Newcastle-Ottawa scale,NOS)对纳入分析的文献进行评价,如有分歧采用第三方意见[9]。按NOS 量表评价内容分8 个给分条目、9 个给分点,每点评1 分:(1)研究人群的选择。病例选择是否恰当?是否有代表性?对照组的选择是否与病例组为同一人群对照?如何确定对照组?每点1 分,共4分。(2)组间可比性。研究设计和统计分析时是否考虑病例组和对照组的可比性,对混杂因素是否控制?年龄、种族、区域、性别、样本结构等均视为重要混杂因素,凡控制一项者评1 分,共2 分。(3)对暴露因素的确定。如何对暴露因素进行确定?是否采取相同的方法确定病例组和对照组的暴露因素?两组的无应答率?每点1 分,共3 分。总评分>6 分的文献认为是高质量。
1.3 统计学处理
采用Review Manager 5.3 软件进行Meta 分析,采用比值比(OR)为效应量,各效应量均以95% CI表示。各纳入研究结果间的异质性采用I2检验,当各研究间异质性可接受(I2<50%)时,采用固定效应模型进行Meta分析;若各研究间存在统计学异质性(I2≥50%),分析其异质性来源,如无临床异质性,采用随机效应模型进行分析。
2 结 果
2.1 病例-对照研究结果分析
本研究共纳入DVT组患者500 例,平均年龄(61.59±13.04)岁。并按病因、性别1:1配对选取500 例无血栓患者作为对照,平均年龄(57.16±16.58)岁。DVT 组患者的平均年龄较对照组患者高,采取独立样本t检验(t=4.7,P <0.01),具有统计学意义。500 例DVT 患者中,O 型血196例(39.2%),非O 型 血304 例(60.8%)。500例非DVT对照组患者中,O型血92例(18.4%),非O型血408例(81.6%)。统计后发现,非O型血较O型血个体血栓发生风险升高(RR=2.859,95% CI=2.142~3.817),经χ2检验后,具有统计学意义(χ2=52.747,P<0.01)(表1)。
考虑到有多种因素可能会影响到DVT 的形成,将500例DVT患者按病因分为无明显诱因者267例(53.4%)、妊娠者3例(0.60%)、外伤者73例(14.60%)、手术者74例、(14.80%)、肿瘤者72 例(14.40%)、长期卧床者11 例(2.20%)。分别计算各组患者特征及血分布,从而排除不同诱因带来的误差(表2)。其中在无明显诱因组、外伤组、手术组中DVT患者较非DVT患者年龄较高,非O型血较O型血发生DVT的可能性增加(均P<0.05)。在癌症患者组只有非O型血与DVT形成有统计学意义(P=0.003)。而在妊娠组及卧床组患者中,年龄及血型在DVT行程中未表现出统计学差异(均P>0.05)。
表1 DVT 组与对照组特征与血型分布比较
Table 1 Comparison of the features and blood group distribution between DVT group and control group
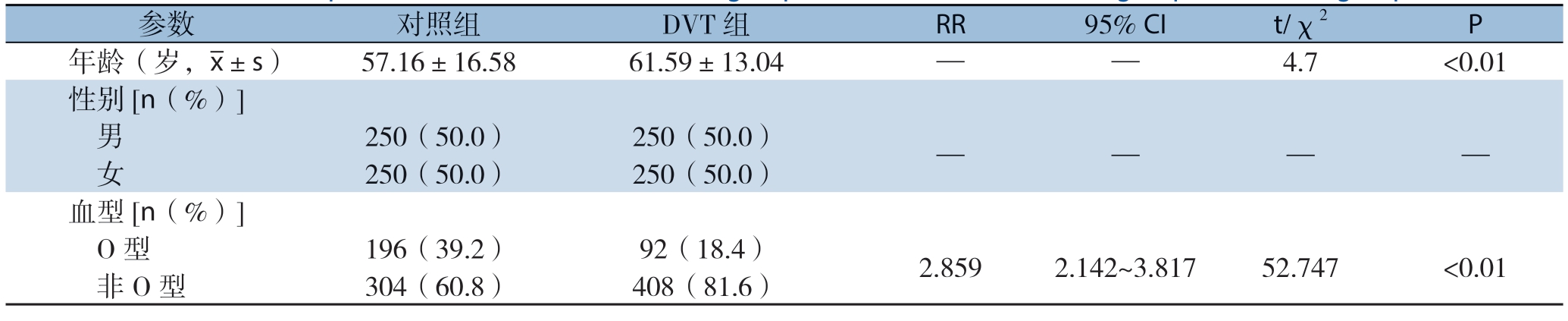
参数 对照组 DVT 组 RR 95% CI t/χ2 P年龄(岁,x±s)57.16±16.58 61.59±13.04 — — 4.7 <0.01性别[n(%)]男 250(50.0)250(50.0)— — — — 女 250(50.0)250(50.0)血型[n(%)]O 型 196(39.2)92(18.4)2.859 2.142~3.817 52.747 <0.01 非O 型 304(60.8)408(81.6)
表2 DVT 组与对照组特征与血型分布的亚组分析
Table 2 Subgroup analysis of the features and blood group distribution between DVT group and control group

参数 对照组 DVT 组 RR 95% CI t/χ2 P无明显诱因 年龄(岁,x±s) 58.18±16.86 62.80±13.10 — — 3.524 <0.01 血型[n(%)]O 型 96(36.0)44(16.5)2.845 1.819~4.282 26.177 <0.01 非O 型 171(64.0)223(83.5)妊娠 年龄(岁,x±s)25.67±3.06 26.33±1.16 — — 0.354 0.742 血型[n(%)]O 型 1(33.3)1(33.3)1 0.034~29.807 0 1 非O 型 2(66.7)2(66.7)外伤 年龄(岁,x±s) 55.14±19.12 59.89±11.51 — — 1.820 0.071 血型[n(%)]O 型 31(42.5)14(19.2)3.111 1.477~6.552 9.284 0.002 非O 型 42(57.5)59(80.8)手术 年龄(岁,x±s) 50.23±15.31 59.11±13.27 — — 3.770 <0.01 血型[n(%)]O 型 31(41.9)16(21.6)2.613 1.271~5.373 7.015 0.008 非O 型 43(58.1)58(78.4)癌症 年龄(岁,x±s)63.50±9.15 62.28±12.12 — —-0.683 0.495 血型[n(%)]O 型 33(45.8)16(22.2)2.962 1.436~6.106 8.940 0.003 非O 型 39(54.2)56(77.8)卧床 年龄(岁,x±s) 59.55±11.09 65.45±11.79 — — 1.211 0.240 血型[n(%)]O 型 4(36.4)1(9.1)5.714 0.528~30.325 2.329 0.127 非O 型 7(63.6)10(90.9)
2.2 Meta 分析结果
2.2.1 检索结果 根据检索策略,排除重复文献,共检索出文献137 篇。经纳入、排除标准检验后,最终纳入文献30 篇(图1),其基本资料见表3。

图1 文献筛选流程图
Figure 1 Literature screening process
表3 纳入文献基本特征(n)
Table 3 General characteristics of the included studies(n)

纳入研究 年份DVT 组 对照组O 型血例数 总人数 O 型血例数 总人数Ahmed,等[10] 2015 46 148 80 148 Bhanvadia,等[11] 2019 27 90 568 1251 Carter,等[8] 2002 153 343 162 343 Cohen,等[12] 2012 32 161 541 1613 Jick,等[13] 1978 16 86 157 344 Li,等[14] 2015 73 434 178 236 Mizrahi,等[15] 2015 14 56 207 467 Nascimento,等[16] 2015 12 44 14 26 Ohira,等[17] 2007 175 492 479 1008 Paiva,等[18] 2009 31 148 130 233 Ribeiro,等[19] 2016 1 158 4 062 2 146 4 659 Robinson,等[20] 1980 37 125 157 333 Shusterman,等[21] 2018 31 75 81 151 Spiezia,等[22] 2013 58 249 108 244 Suchon,等[23] 2016 227 968 323 874 Sun,等[24] 2017 340 1 412 60 118199 248 Sun,等[25] 2015 60 214 286 636 Teixeira,等[26] 2009 52 175 98 175 Tufano,等[27] 2013 19 77 1 900 4 272 van Adrichem,等[28] 2015 1 024 3 682 2 220 4 657 van Langevelde,等[29] 2011 1 130 3 925 2 149 4 667白璐[30] 2016 25 154 41 154郭海[31] 2017 5 34 38 110齐典文,等[32] 2014 3 24 28 66王美堂,等[33] 2004 8 57 45 128王燕玲,等[34] 2017 71 181 25 93席少枝[35] 2012 8 48 14 48于连有[36] 2016 21 30 12 30赵海歌[37] 2017 14 73 56 146周稳,等[38] 2015 21 30 52 82合计 5 111 18 309 72 767227 154
2.2.2 纳入文献的质量评价 采用NOS 量表对纳入的文献进行质量评价,各纳入文献总评分均>6 分,为高质量文献(表4)。
表4 纳入文献NOS 量表
Table 4 The NOS scale of the included studies
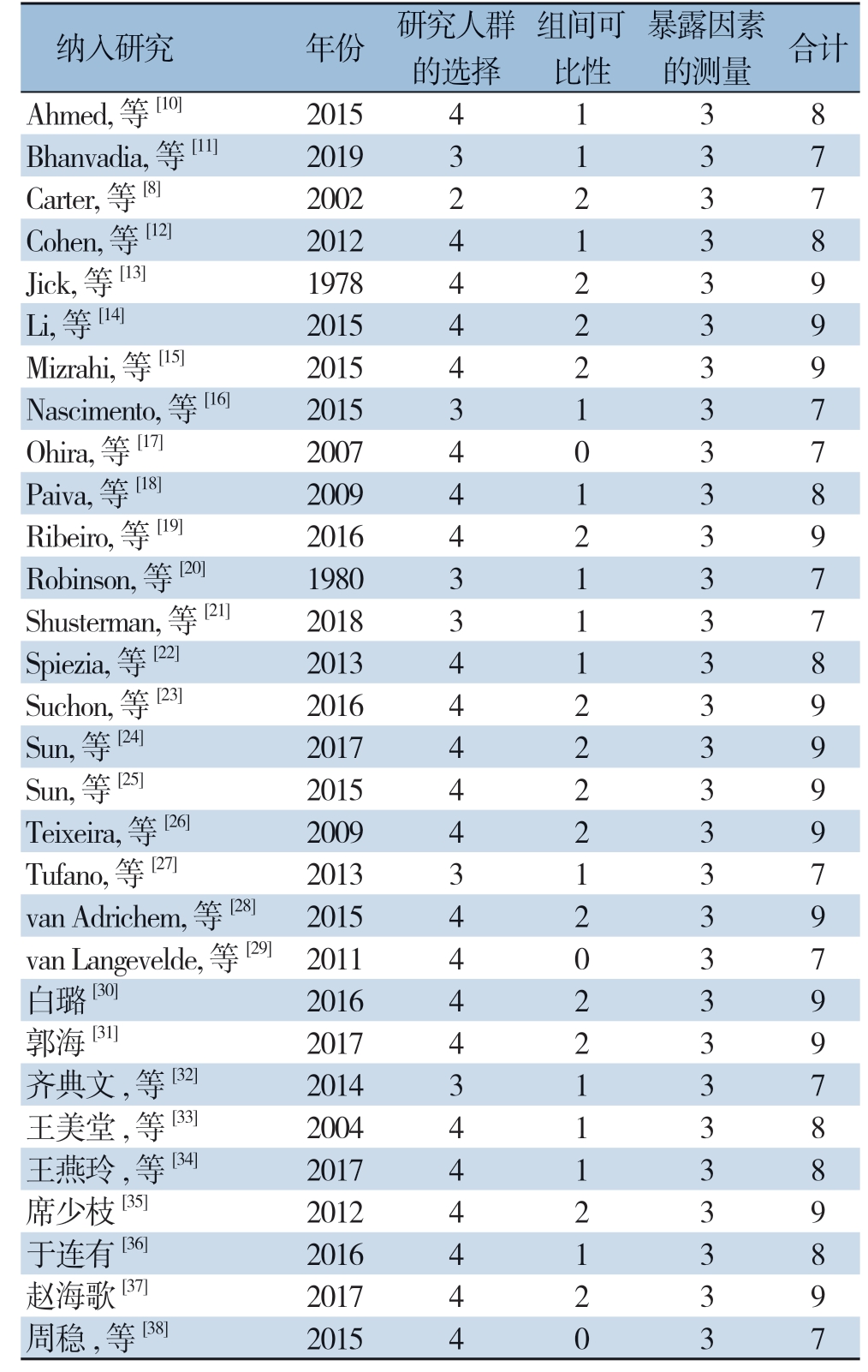
纳入研究 年份 研究人群的选择组间可比性暴露因素的测量 合计Ahmed,等[10] 2015 4 1 3 8 Bhanvadia,等[11] 2019 3 1 3 7 Carter,等[8] 2002 2 2 3 7 Cohen,等[12] 2012 4 1 3 8 Jick,等[13] 1978 4 2 3 9 Li,等[14] 2015 4 2 3 9 Mizrahi,等[15] 2015 4 2 3 9 Nascimento,等[16] 2015 3 1 3 7 Ohira,等[17] 2007 4 0 3 7 Paiva,等[18] 2009 4 1 3 8 Ribeiro,等[19] 2016 4 2 3 9 Robinson,等[20] 1980 3 1 3 7 Shusterman,等[21] 2018 3 1 3 7 Spiezia,等[22] 2013 4 1 3 8 Suchon,等[23] 2016 4 2 3 9 Sun,等[24] 2017 4 2 3 9 Sun,等[25] 2015 4 2 3 9 Teixeira,等[26] 2009 4 2 3 9 Tufano,等[27] 2013 3 1 3 7 van Adrichem,等[28] 2015 4 2 3 9 van Langevelde,等[29] 2011 4 0 3 7白璐[30] 2016 4 2 3 9郭海[31] 2017 4 2 3 9齐典文,等[32] 2014 3 1 3 7王美堂,等[33] 2004 4 1 3 8王燕玲,等[34] 2017 4 1 3 8席少枝[35] 2012 4 2 3 9于连有[36] 2016 4 1 3 8赵海歌[37] 2017 4 2 3 9周稳,等[38] 2015 4 0 3 7
2.2.3 Meta 分析结果 在纳入的30 篇文献中,DVT 组O型血4891 例(27.79%),对照组O 型血72413 例(31.98%),经异质性分析,整体存在异质性(I2=87%,P<0.01),采取随机效应模型,Meta 分析结果显示O 型血较非O 血型在DVT 发生风险上差异存在统计学意义(RR=0.62,95% CI=0.56~0.69,P<0.05)(图2)。
2.2.4 发表偏倚分析 绘制倒置漏斗图发现,纳入的30 篇文献完整地出现在图上,各亚组以合并效应量RR 值为中心散开分布,基本对称,小样本的效应点基本分布在底部,大样本逐渐趋于在上部一个较窄的范围内,呈倒置漏斗形(图3)。
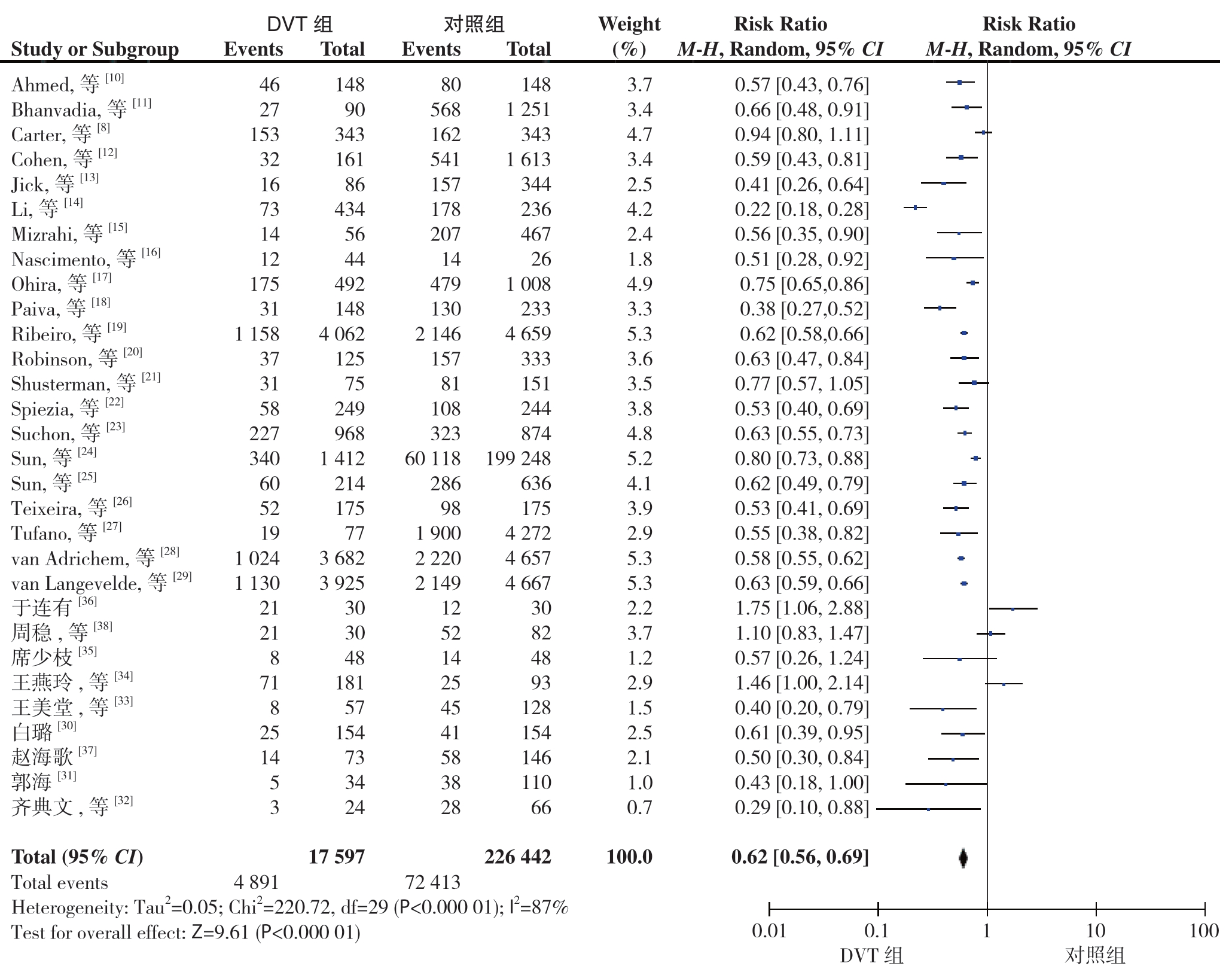
图2 森林图
Figure 2 The forest plot
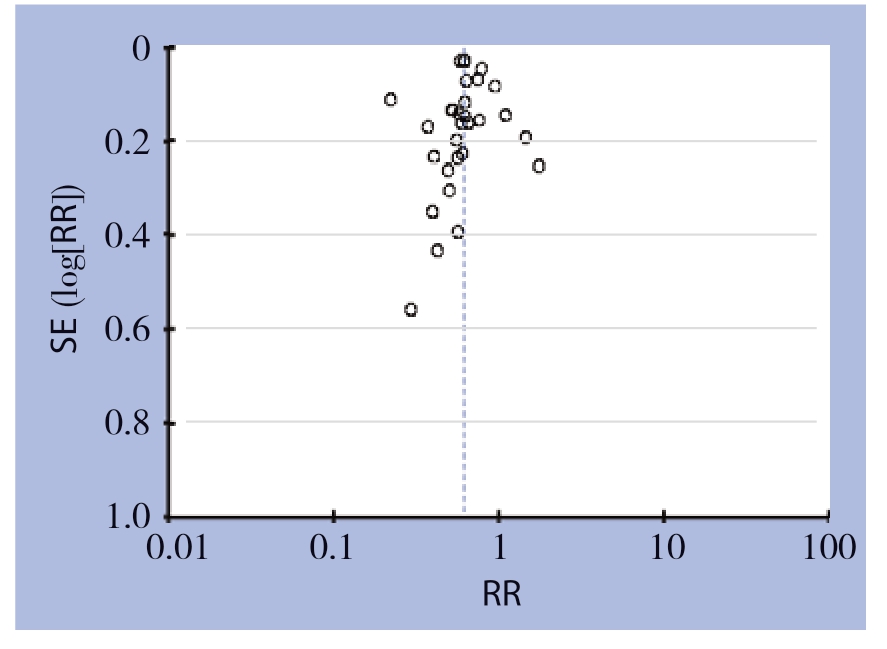
图3 漏斗图
Figure 3 The funnel plot
3 讨 论
ABO血型系统的抗原(A、B和H)由置于红细胞膜外表面的复杂碳水化合物分子组成[39]。其抗原基因位于9号染色体长臂(9q34.2),但并不是染色体直接编码抗原。ABO抗原是从共同的前体物质加工而来的。前体物质会在岩藻糖基转移酶的催化下形成H抗原,即O型血个体。然后在各自催化酶的作用下加上不同的基团形成A、B型血[40],所以在结构上非O型血个体的血型抗原较O型血个体复杂,可能产生不同的生理功能。
DVT是住院患者中发病率比较高的一类疾病[41]。目前,临床上治疗DVT的患者时,通常是询问有没有长期卧床、手术、外伤、妊娠、癌症等病史,而在预防DVT形成方面,也同样是重点针对这些方面。但是DVT形成在病因学上是多样性的,除了继发性因素外,还有许多原发性因素包括抗凝血酶缺乏症、因子VII缺乏症、纤溶酶原缺乏症、因子V Leiden突变、凝血酶原基因G20210A突变、蛋白C缺乏症、蛋白S缺乏症、高半胱氨酸血症等[42]。因此该疾病个体差异较大,无明显诱因的患者仍占大多数。
归因于DVT 病因学的复杂性,目前关于ABO 血型系统对DVT 的影响仍有争论,且A B O血型与DVT形成之间关系的机制尚不清楚。有研究[43-44]表明,ABO 血型系统与血管性血友病(Von Willebr and,VWF)的水平密切相关。Schleef等[45]研究显示,O型血人群的vWF水平为654~1028 U/L,而非O型血人群其vWF水平为900~1390 U/L,平均水平为1339 U/L。
vWF是由内皮细胞、巨核细胞分泌的一种分子量不等的多聚体,可以通过介导血小板与内皮下胶原的黏附反应、介导血小板与血小板之间的聚集、作为凝血因子Ⅷ的保护性载体来促进血栓形成。vWF会在金属蛋白酶ADAMTS13的催化下裂解,最终成为没有功能的蛋白水解片段。
ABO抗原系统影响血栓形成的机制可能在于其抗原通过寡糖链存在于vWF之上,不同血型的寡糖链不同,会影响到vWF结构的空间位阻和电荷效应,从而会影响金属蛋白酶ADAMTS13的作用,进而影响裂解速率[46-47]。另外vWF起初是以大型复合物的形式存在的,当内皮受损后,紧密折叠的vWF会在血流的作用下变疏松,暴露作用基团,产生生物活性。寡糖链的不同,可能会影响vWF结构的变化速率。
本研究通过病例对照研究发现对于无明显诱因、外伤、手术、癌症的患者ABO抗原系统与DVT发生之间存在相关性。而对于妊娠及长期卧床患者未能证明相关性,考虑到妊娠及卧床患者病例数目较少,该结论有待进一步扩大样本进行验证。通过纳入30篇临床对照研究进行的Meta分析也进一步证实了O型血对DVT患者的保护作用,差异有统计学意义。
综上所诉,于无明显诱因、外伤、手术、癌症的患者将ABO血型纳入DVT危险因素的综合分析中,对于血栓的个体化预防及精准治疗有一定临床价值。对于妊娠组及长期卧床组患者,ABO血型的不一定能表现出足够临床价值。考虑到妊娠及卧床患者病例数目较少,结论仍需进一步验证。
[1]朱岩举,党晓卫,许培钦.血栓性疾病诊断及防治研究的进展[J].中国普通外科杂志,2010,19(6):680-682.
Zhu YJ,Dang XW,Xu PX.Recent research progress on diagnosis and prevention of thrombotic diseases 680[J].Chinese Journal of General Surgery,2010,19(6):680-682.
[2]Chung I,Lip GY.Virchow's triad revisited:blood constituents[J].Pathophysiol Haemost Thromb,2003/2004,33(5/6):449-454.doi:10.1159/000083844.
[3]张钦辉.临床输血学[M].上海:上海科学技术出版社,2000:51-52.
Zhang QH.Clinical blood transfusion[M].Shanghai:Shanghai Scientific& Technical Publishers,2000:51-52
[4]郭忠武,薛英威.胃癌患者ABO血型与临床病理特征关系[J].中国普通外科杂志,2015,24(10):1367-1371.doi:10.3978/j.issn.1005-6947.2015.10.005.Guo ZW,Xue YW.Relations of ABO blood group with clinicopathologic features of patients with gastric cancer[J].Chinese Journal of General Surgery,2015,24(10):1367-1371.doi:10.3978/j.issn.1005-6947.2015.10.005.
[5]Jick H,Slone D,Westerholm B,et al.Venous thromboembolic disease and ABO blood type.A cooperative study[J].Lancet,1969,1(7594):539-542.doi:10.1016/s0140-6736(69)91955-2.
[6]Gándara E,Kovacs MJ,Kahn SR,et al.Non-OO blood type infl uences the risk of recurrent venous thromboembolism.A cohort study[J].Thromb Haemost,2013,110(6):1172-1179.doi:10.1160/TH13-06-0488.
[7]Koster T,Blann AD,Briët E,et al.Role of clotting factor VIII in effect of von Willebrand factor on occurrence of deep-vein thrombosis[J].Lancet,1995,345(8943):152-155.doi:10.1016/s0140-6736(95)90166-3.
[8]Carter YM,Caps MT,Meissner MH.Deep venous thrombosis and ABO blood group are unrelated in trauma patients[J].J Trauma,2002,52(1):112-116.doi:10.1097/00005373-200201000-00019.
[9]Stang A.Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in metaanalyses[J].Eur J Epidemiol,2010,25(9):603-605.doi:10.1007/s10654-010-9491-z.
[10]Ahmed SG,Kagu MB,Ibrahim UA,et al.Impact of sickle cell trait on the thrombotic risk associated with non-O blood groups in northern Nigeria[J].Blood Transfus,2015,13(4):639-643.doi:10.2450/2015.0335-14.
[11]Bhanvadia S,Kazerouni K,Bazargani ST,et al.Validating the role of ABO blood type in risk of perioperative venous thromboembolism after radical cystectomy[J].World J Urol,2019,37(1):173-179.doi:10.1007/s00345-018-2351-2.
[12]Cohen W,Castelli C,Alessi MC,et al.ABO blood group and von Willebrand factor levels partially explained the incomplete penetrance of congenital thrombophilia[J].Arterioscler Thromb Vasc Biol,2012,32(8):2021-2028.doi:10.1161/ATVBAHA.112.248161.
[13]Jick H,Porter J.Thrombophlebitis of the lower extremities and ABO blood type[J].Arch Intern Med,1978,138(10):1566-1567.
[14]Li D,Pise MN,Overman MJ,et al.ABO non-O type as a risk factor for thrombosis in patients with pancreatic cancer[J].Cancer Med,2015,4(11):1651-1658.doi:10.1002/cam4.513.
[15]Mizrahi T,Leclerc JM,David M,et al.ABO Group as a Thrombotic Risk Factor in Children With Acute Lymphoblastic Leukemia:A Retrospective Study of 523 Patients[J].J Pediatr Hematol Oncol,2015,37(5):e328-332.doi:10.1097/MPH.0000000000000333.
[16]Nascimento NM,Bydlowski SP,Soares RP,et al.ABO blood group in primary antiphospholipid syndrome:influence in the site of thrombosis?[J].J Thromb Thrombolysis,2015,40(3):374-378.doi:10.1007/s11239-015-1176-8.
[17]Ohira T,Cushman M,Tsai MY,et al.ABO blood group,other risk factors and incidence of venous thromboembolism:the Longitudinal Investigation of Thromboembolism Etiology(LITE)[J].J Thromb Haemost,2007,5(7):1455-1461.doi:10.1111/j.1538-7836.2007.02579.x.
[18]Paiva SG,Sabino AP,Carvalho MG,et al.Polymorphisms in exons 6 and 7 of the ABO locus and their association with venous thrombosis in young Brazilian patients[J].Blood Coagul Fibrinolysis,2009,20(2):122-128.doi:10.1097/MBC.0b013e328323da99.
[19]Ribeiro DD,Lijfering WM,Rosendaal FR,et al.Risk of venous thrombosis in persons with increased body mass index and interactions with other genetic and acquired risk factors[J].J Thromb Haemost,2016,14(8):1572-1578.doi:10.1111/jth.13371.
[20]Robinson WM,Roisenberg I.Venous thromboembolism and ABO blood groups in a Brazilian population[J].Hum Genet,1980,55(1):129-131.doi:10.1007/BF00329140.
[21]Shusterman M,Golub E,Mowrey WB,et al.The association between ABO blood types and venous thromboembolism in individuals with a positive antiphospholipid profile is varied by sex[J].Lupus,2018,27(2):319-326.doi:10.1177/0961203317721352.
[22]Spiezia L,Campello E,Bon M,et al.ABO blood groups and the risk of venous thrombosis in patients with inherited thrombophilia[J].Blood Transfus,2013,11(2):250-253.doi:10.2450/2012.0060-12.
[23]Suchon P,Al Frouh F,Henneuse A,et al.Risk factors for venous thromboembolism in women under combined oral contraceptive.The PILl Genetic RIsk Monitoring(PILGRIM)Study[J].Thromb Haemost,2016,115(1):135-142.doi:10.1160/TH15-01-0045.
[24]Sun X,Feng J,Wu W,et al.ABO blood types associated with the risk of venous thromboembolism in Han Chinese people:A hospital-based study of 200,000 patients[J].Sci Rep,2017,7:42925.doi:10.1038/srep42925.
[25]Sun Y,Mao P,Lu J,et al.ABO blood type and ABO gene with susceptibility to deep vein thrombosis following orthopedic surgery:a case-control study in Chinese Han population[J].Sci China Life Sci,2015,58(4):390-391.doi:10.1007/s11427-015-4819-2.
[26]Teixeira Mello TB,Machado TF,Montavão SA,et al.Assessing the coagulation factor levels,inherited thrombophilia,and ABO blood group on the risk for venous thrombosis among Brazilians[J].Clin Appl Thromb Hemost,2009,15(4):408-414.doi:10.1177/1076029607311777.
[27]Tufano A,Coppola A,Nardo A,et al.Non-O blood group as a risk factor for cerebral vein thrombosis[J].Thromb Haemost,2013,110(1):197-199.doi:10.1160/TH13-02-0112.
[28]van Adrichem RA,Nelissen RG,et al.Risk of venous thrombosis after arthroscopy of the knee:results from a large population-based case-control study[J].J Thromb Haemost,2015,13(8):1441-1448.doi:10.1111/jth.12996.
[29]van Langevelde K,Lijfering WM,Rosendaal FR,et al.Increased risk of venous thrombosis in persons with clinically diagnosed superfi cial vein thrombosis:results from the MEGA study[J].Blood,2011,118(15):4239-4241.doi:10.1182/blood-2011-05-356071.
[30]白璐.中老年外伤性人工髋关节置换术后合并下肢深静脉血栓危险因素分析[D].唐山:华北理工大学,2016:1-63.
Bai L.Risk Factors Analysis of Deep Venous ThrombosisAfter Hip Arthroplasty in The Elderly Population[D].Tangshan:North China University of Science and Technology,2016:1-63.
[31]郭海.胸外科肺癌患者围手术期高凝状态合并静脉血栓栓塞的临床试验研究[D].南宁:广西医科大学,2017.
Guo H.Clinical Study of Hypercoagulable State Withvenous Theombosis during the perioperative of Lung Carcinomain Thoracic Surgery Department[D].Nanning:Guangxi Medical University,2017.
[32]齐典文,张国川,扈文海,等.骨转移癌患者下肢深静脉血栓形成的危险因素分析[J].中华肿瘤杂志,2014,36(6):469-472.doi:10.3760/cma.j.issn.0253-3766.2014.06.016.
Qi DW,Zhang GC,Hu WH,et al.Analysis of risk factors for deep vein thrombosis of the lower extremity in patients with bone metastases[J].Chinese Journal of Oncology,2014,36(6):469-472.doi:10.3760/cma.j.issn.0253-3766.2014.06.016.
[33]王美堂,姚小鹏,李强.肺血栓栓塞症和深静脉血栓形成住院患者相关危险因素的分析[J].第二军医大学学报,2004,25(7):740-742.doi:10.3321/j.issn:0258-879X.2004.07.013.
Wang MT,Yao XP,Li Q.Risk factor analysis of hospitalized patients with pulmonary thromboembolism and deep venous thrombosis[J].Academic Journal of Second Military Medical University,2004,25(7):740-742.doi:10.3321/j.issn:0258-879X.2004.07.013.
[34]王燕玲,何丽,王燕燕,等.非小细胞肺癌合并静脉血栓栓塞症危险因素分析[J].中国医学前沿杂志:电子版,2017,9(8):126-129.doi:10.12037/YXQY.2017.08-29.
Wang YL,He L,Wang YY,et al.Risk factors of non-small cell lung cancer complicated with venous thromboembolism[J].Chinese Journal of the Frontiers of Medical Science:Electronic Version,2017,9(8):126-129.doi:10.12037/YXQY.2017.08-29.
[35]席少枝.自发性静脉血栓栓塞症实验室早期诊断指标及遗传易感因素的筛查分析[D].北京:军医进修学院,2012.
Xi SZ.Screening for the early diagnostic laboratory index and genetic susceptibility gene of idiopathic venous thromboembolism[D].Beijing:PLA Postgraduate Medical School,2012.
[36]于连有.癌症骨转移患者发生下肢深静脉血栓的影响因素研究[J].中国实验诊断学,2016,20(3):402-405.
Yu LY.Influencing Factors if Deep Vein Thrombosis in Parients with Cancer with Bone Metastases[J].Chinese Journal of Laboratory Diagnosis,2016,20(3):402-405.
[37]赵海歌.ABO血型、vWF和凝血因子Ⅷ与肺血栓栓塞相关性的研究[D].保定:河北大学,2017.
Zhao HG.Relationship between ABO blood type,VWF,coagulation factors Ⅷ and pulmonary thromboembolism[D].Baoding:Hebei University,2017.
[38]周稳,叶斌,任冬.骨转移癌患者发生下肢深静脉血栓的相关因素分析[J].中国肿瘤临床与康复,2015,22(6):681-683.doi:10.13455/j.cnki.cjcor.2015.06.14.
Zhou W,Ye B,Ren D.Analysis of related factors of deep venous thrombosis of lower limbs in cancer patients with bone me-tastases[J].Chinese Journal of Clinical Oncology and Rehabilitation,2015,22(6):681-683.doi:10.13455/j.cnki.cjcor.2015.06.14.
[39]Storry JR,Olsson ML.The ABO blood group system revisited:a review and update[J].Immunohematology,2009,25(2):48-59.
[40]Lowe JB.The blood group-specific human glycosyltransferases[J].Baillieres Clin Haematol,1993,6(2):465-492.doi:10.1016/s0950-3536(05)80155-6.
[41]Muellner SK,Haut ER,Streiff MB,et al.ABO blood group as a potential risk factor for venous thromboembolism in acutely injured patients[J].Thromb Haemost,2011,105(1):5-13.doi:10.1160/TH10-08-0504.
[42]Heit JA.Risk factors for venous thromboembolism[J].Clin Chest Med,2003,24(1):1-12.doi:10.1016/s0272-5231(02)00077-1.
[43]Moeller A,Weippert-Kretschmer M,Prinz H,et al.Influence of ABO Blood Groups on Primary Hemostasis[J].Transfusion,2001,41(1):56-60.doi:10.1046/j.1537-2995.2001.41010056.x.
[44]Preston AE.The Plasma Concentration of Factor VIII in the Normal Population[J].Br J Haematol,1964,10:110-114.doi:10.1111/j.1365-2141.1964.tb00683.x.
[45]Schleef M,Strobel E,Dick A,et al.Relationship between ABO and Secretor genotype with plasma levels of factor VIII and von Willebrand factor in thrombosis patients and control individuals[J].Br J Haematol,2005,128(1):100-107.doi:10.1111/j.1365-2141.2004.05249.x.
[46]Furlan M,Robles R,Lämmle B.Partial purification and characterization of a protease from human plasma cleaving von Willebrand factor to fragments produced by in vivo proteolysis[J].Blood,1996,87(10):4223-4234.
[47]Sodetz JM,Paulson JC,McKee PA.Carbohydrate composition and identification of blood group A,B,and H oligosaccharide structures on human Factor VIII/von Willebrand factor[J].J Biol Chem,1979,254(21):10754-10760.
