肝细胞癌(hepatocellular carcinoma,HCC)伴胆管癌栓(bile duct tumor thrombus,BDTT)较为少见,发生率约0.5%~12.9%[1-6]。外科手术是HCC伴BDTT首选的治疗方式[7-10],但是否保留肝外胆管还存在争议[11-13]。
由于BDTT在肝外胆管膨胀性生长的特性,较少侵犯肝外胆管壁,大部分可以行保留肝外胆管的取栓术[14-16]。关于如何取出肝外BDTT的相关研究较少,目前主要方法有:胆管切开取栓、剥离技术(peeling off technique)、内镜下取栓等[17-20]。但以上方法并不符合肿瘤无瘤原则。近来,笔者单位总结出一种安全、有效、且符合无瘤原则的取栓方法,命名为“q”形胆管切开取栓术。本研究回顾性总结2019年3月我科收治的1例HCC伴BDTT患者的临床资料,探讨“q”形胆管切开取栓术的方法和临床疗效。
1 资料与方法
1.1 一般资料
患者 男性,37岁,身高156cm,体质量52 kg。以“发现眼黄半年余,加重伴右上腹闷痛1月”为主诉于2019年3月24日入院。患者无畏冷发热。既往吸烟18年,无酗酒史。体格检查:全身皮肤、巩膜重度黄染,右上腹深压痛,无反跳痛,余腹无压痛、反跳痛,余无明显阳性体征。实验室检查:血常规正常,肝功能:TBIL 311.08 μmol/L、DBIL 159.7 μmol/L、Alb 39g/L、ALT 58 U/L、AST 61 U/L、GGT 208 U/L、ALP 313.0 U/L。肿瘤标志物:CA19-9128.40 U/mL、AFP 185.0 ng/mL。乙肝两对半提示:乙肝“小三阳”。心电图正常,胸部CT无异常。上腹部MRI平扫及增强(图1):⑴肝右后叶下段(S6段)占位性病变,约3.9 cm ×2.9 cm ×3.0 cm,考虑恶性肿瘤。⑵肝硬化多发再生结节形成,部分为异形增生结节。⑶肝门区肿大的淋巴结,约2.0 cm×1.8 cm×2.1 cm,并肝内管扩张,邻近门脉右支受压。⑷慢性胆囊炎改变。本研究通过我院医学伦理委员会审批,患者及家属术前均签署知情同意书。
1.2 术前评估
1.2.1 可切除性评估 根据MRI 检查结果,患者诊断为HCC 伴BDTT(BCLC 分期A 期,中国原发性肝癌诊疗规范分期Ia 期)。依据日本肝癌研究小组BDTT 分型(B0 型:未发现BDTT;B1 型:癌栓位于三级胆管及以上;B2 型:癌栓位于二级胆管;B3 型:癌栓位于一级胆管;B4 型:癌栓位于肝外胆管),该病例为HCC 伴B4 型BDTT。肿瘤位于右肝后叶,门静脉及肝静脉无肉眼癌栓。
1.2.2 肝脏储备功能评估 考虑重度梗阻性黄疸,入院后立即在B 超引导下行右肝胆管PTCD 置管引流术。经过16 d 引流减黄,复查肝功能为TBIL 141.20 μmol/L、DBIL 127 μmol/L、ALB 38 g/L、ALT 40 U/L、AST 55 U/L。通过三维重建肝脏体积测定:左半肝为736.94 mL,残余肝体积约占标准肝体积的42.84%,可耐受右半肝切除。
1.2.3 全身情况评估 患者一般情况与营养状况良好,无合并高血压、糖尿病、心脏病等基础疾病。
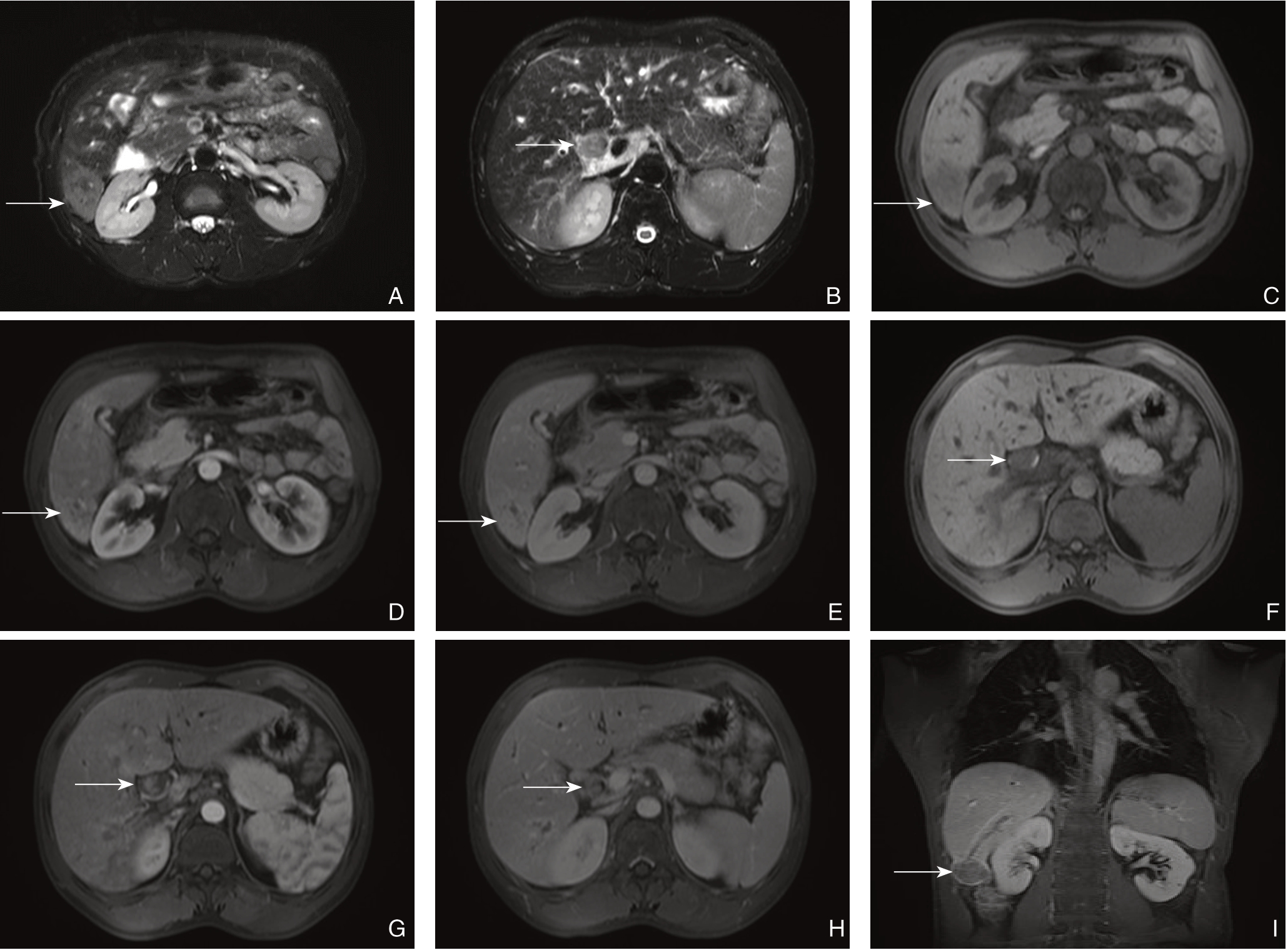
图1 影像学资料 A:MRI 检查示T2WI 右肝肿瘤呈高信号(箭头所示);B:MRI 检查示T2WI 见胆总管癌栓呈稍高信号(箭头所示);C:MRI 检查T1WI 示右肝肿瘤呈低信号(箭头所示);D:MRI 检查示动脉期右肝肿瘤呈不均匀强化(箭头所示);E:MRI 检查示静脉期右肝肿瘤呈等信号(箭头所示);F:MRI 检查示T1WI 见胆总管癌栓呈低信号(箭头所示);G:MRI 检查示动脉期见胆总管癌栓不均匀强化(箭头所示);H:MRI 检查示静脉期见胆总管癌栓呈低信号(箭头所示);I:MRI 检查示右肝VI 段肿瘤与胆道癌栓相连(箭头所示)
Figure 1 Imaging data A:MRI showing hyperintensity of the right liver tumor on T2WI (shown by arrow);B:MRI showing mild hyperintensity of the common bile duct tumor thrombus on T2WI (shown by arrow);C:MRI showing hypointensity of the right liver tumor on T1WI signal (shown by arrow);D:MRI showing uneven enhancement of the right liver tumor in arterial phase (shown by arrow);E:MRI showing isointensity of the right liver tumor in venous phase (shown by arrow);F:MRI showing hypointensity of the common bile duct tumor thrombus on T1WI (shown by arrow);G:MRI showing uneven enhancement of the common bile duct tumor thrombus in arterial phase (shown by arrow);H:MRI showing hypointensity of the common bile duct tumor thrombus in venous phase (shown by arrow);I:MRI showing connection between the segment 6 tumor with the bile duct tumor thrombus (shown by arrow)
1.3 手术方法
根据术前影像学及肝功能评估,患者拟行右半肝切除+胆囊切除+“q”形胆管切开取栓+肝十二指肠韧带淋巴结清扫术。手术步骤:⑴切口与探查:患者取仰卧位,常规气管插管,全身麻醉。取右上腹肋缘下反“L”切口,探查胆囊,胰腺,脾脏,胃,结肠,腹膜及盆腔无转移灶。⑵术中B超检查定位:通过术中B超检查肝脏,肿瘤位于右肝后叶VI段,外生型,大小约4 cm×3 cm×3 cm。胆总管明显扩张,约2.5 cm,内有癌栓,张力较高。同时B超定位下标识肝中静脉,避免右半肝切除时损伤肝中静脉。⑶前入路切除右半肝:分离胆囊三角,顺逆结合切除胆囊。超声刀离断肝圆韧带,镰状韧带,左冠状韧带及右冠状韧带部分,显露肝静脉陷窝及右肝静脉右侧壁。解剖第一肝门,离断右肝动脉、门静脉右支,循肝中静脉前入路切除右半肝,离断并缝扎右肝静脉,离断肝周韧带,仅剩右肝胆管与右半肝相连。⑷“q”形胆总管切开取栓:游离显露出胆总管、肝总管,以电刀纵行切开胆总管前壁至右肝胆管前壁,长约4 cm(图2A)。可见胆总管癌栓弹出胆总管(图2B)。环行切断右肝胆管汇入肝总管处,呈“q”形,一体化切除右半肝及肝外BDTT(图2C)。右肝胆管断端冰冻切缘阴性。胆道镜探查胆总管内壁光滑,未见结节及肿物。4-0可吸收缝线连续缝合右肝胆管断端及胆总管前壁(图2D)。冲洗腹腔,未见活动性出血及胆汁漏。右肝断面放置腹腔引流管1根后关腹。手术示意图见图3。
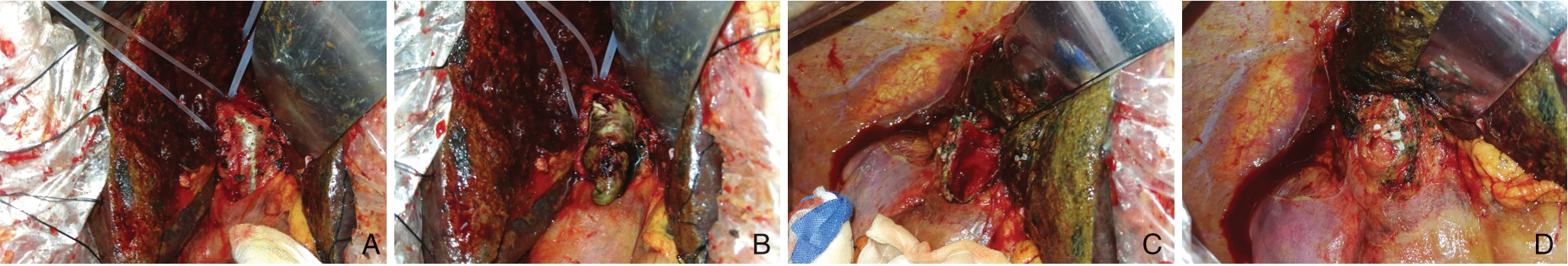
图2 术中图片 A:分离显露胆总管前壁;B:纵行切开胆总管,胆管癌栓自行脱出;C:完整取出胆管癌栓后,探查见胆总管黏膜光滑,无残余癌栓;D:连续缝合胆总管前壁
Figure 2 Intraoperative views A:Dissociation and exposure of the anterior wall of the common bile duct;B:Longitudinal incision of the common bile duct and then spontaneous falling out of the bile duct tumor thrombus;C:After the complete removal of the bile duct tumor thrombus,seeing smooth the bile duct mucosa without tumor thrombus after exploration;D:Closure with continuous suture of the anterior wall of the common bile duct
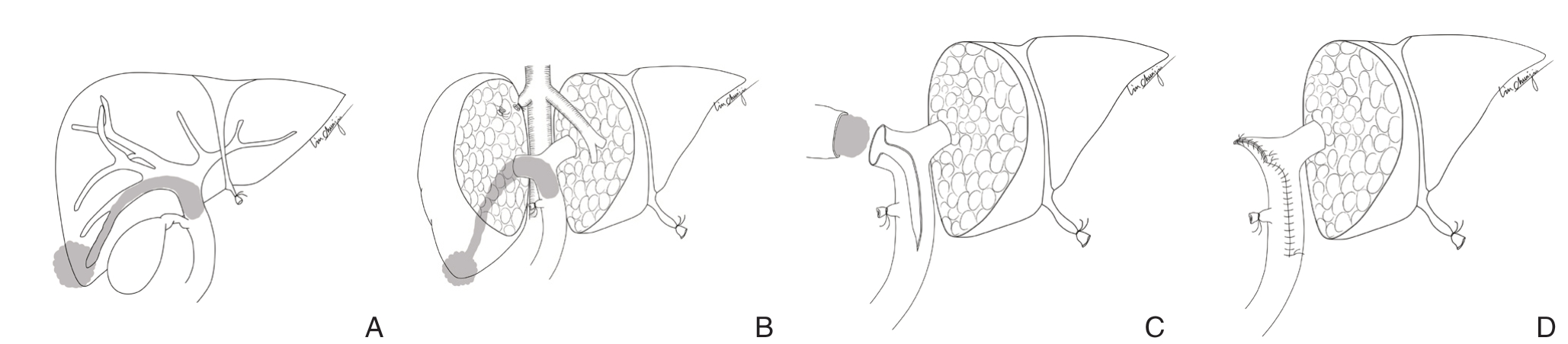
图3 手术示意图 A:肿瘤位于右肝后叶VI 段,呈外生型,癌栓沿右后支胆管延伸至胆总管;B:解剖右肝蒂,离断结扎右肝动脉及门静脉右支,循肝中静脉前入路切除右半肝,离断右肝静脉,离断肝周韧带,仅剩右肝胆管与右半肝相连;C:沿胆总管及右肝管前壁纵行切开,环行切断右肝胆管汇入肝总管处(“q”形取栓术);D:连续缝合右肝胆管断端及胆总管前壁
Figure 3 Schematic diagram A:The lesion locating at the segment VI and the bile duct tumor thrombus extended to the common bile duct;B:Dissecting the right hepatic pedicle,division of the right hepatic artery and right portal vein,hepatic parenchymal resection along the middle hepatic vein and down to the anterior surface of inferior vena cava,and after parenchymal resection,the right hepatic vein was divided,leaving alone the right hepatic duct connected to the common bile duct;C:Longitudinal incision cranially up to the right hepatic duct and caudally down to the tip of the BDTT,plus with a circular incision of the right hepatic duct near the bifurcation(“q-type” biliary thrombectomy;D:Closure of the bile duct stump and common bile duct with continuous suture
1.4 观察指标
观察患者手术时间、术中出血量、术中输血情况、术后并发症(Clavien-Dindo分级)、引流管拔除时间、住院时间、病理学检查结果、随访情况。
1.5 随访
采用门诊及电话方式进行随访,随访内容为患者生活质量和肿瘤复发治疗情况,随访时间截至2020年6月。
2 结果
2.1 手术情况
该患者顺利完成右半肝切除+胆囊切除+“q”形胆管切开取栓+肝十二指肠韧带淋巴结清扫术。手术时间为313 min,术中出血量为150 mL,未输血。术中成功采用“q”形切开胆管完整取出癌栓。
2.2 围术期情况
患者术后恢复顺利,无胆瘘、腹腔感染、肝衰竭等并发症发生,术后第6天拔除腹腔引流管,术后第7天出院。
2.3 病理学检查
剖视右肝肿物及肝内胆管可见癌栓沿着右肝后叶胆管生长,进入右肝胆管及胆总管(图4A)。右肝肿物标本大小为4 cm×3 cm×3 cm,肝原发性结节型低分化肝细胞癌,侵及肝被膜,可见脉管内癌栓。周边肝细胞轻度水肿,间质纤维增生,汇管区中量慢性炎症细胞浸润(图4B-C)。另送(第12组)淋巴结10枚,未见癌转移。胆总管癌栓大小为6.0 cm×2.5 cm×1.5 cm,送检癌组织见肝细胞性肝癌。
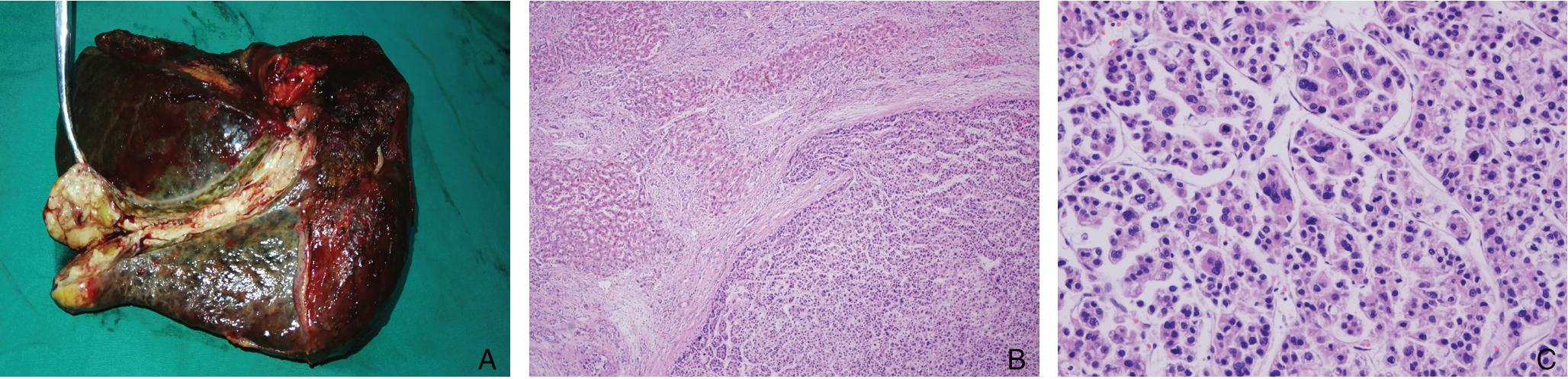
图4 术后图片和病理 A:大体病理标本;B:肝原发性低分化HCC(HE×50);C:肝原发性低分化HCC(HE×200)
Figure 4 Postoperative pathology A:Gross pathological specimen;B:Primary poorly differentiated HCC (HE×50);C:Poorly differentiated HCC (HE×200)
2.4 随访
术后随访14个月患者生活质量良好,肿瘤无复发。
3 讨论
外科手术是HCC伴BDTT的首选治疗方式。日本肝癌研究小组根据BDTT累及胆管不同,将BDTT分为5型,B1~B3型BDTT位于一级胆管以上,解剖性切除肿瘤的同时一并切除了BDTT。B4型BDTT位于肝外胆管,除了需要行半肝切除外,还须行胆总管切开取栓或肝外胆管切除和重建。
对于B4型BDTT是否切除肝外胆管,目前仍存在较大的争议。Wong等[11]报道了37例BDTT患者与222例不伴有BDTT的HCC患者(1:6比例配对)的手术方式及术后并发症的对比,结果显示HCC伴BDTT患者往往实施大面积肝切除、胆肠吻合,且术后并发症较多,但是两者1、3、5年的生存率差异无统计学意义,且该研究认为BDTT不是影响预后的危险因素。因而主张大面积肝切除和肝外胆管切除重建作为HCC伴BDTT的标准术式。韩国和日本32家多中心研究,总共257例B3和B4型HCC伴BDTT患者,Cox比例风险模型证实TNM分期及肝纤维化或肝硬化是影响HCC伴BDTT患者长期生存率的独立预测因子[21]。半肝及以上肝切除联合肝外胆管切除重建能明显提高患者总体生存率,降低术后复发率。因此,该研究强烈推荐对B3、B4型BDTT患者应该积极手术,实施大面积肝切除联合肝外胆管切除,以提高R0切除率。而且单纯的切开取栓存在局部复发和肿瘤腹腔种植的风险[22-23]。
目前,也有不少研究支持保留肝外胆管。首先,BDTT在肝外胆管内呈膨胀性的生长,侵犯肝外胆管壁的情况较为少见[21,24-25]。Shiomi等[24]认为只有BDTT与肝外胆管粘连致密难以切除时,才考虑肝外胆管的切除和重建。该研究证实无论是胆总管切开取栓还是肝外胆管切除,两者间生存率差异无统计学意义。其次,肝外胆管并不是肿瘤术后复发的好发部位。Orimo等[12]报道了42例行肝切除和胆总管切开取栓的HCC伴BDTT患者,其中24例患者术后复发,但仅有1例出现胆总管复发,其余主要是肝内复发及肺转移(肝内复发15例,肺转移3 例,肝脏与肺同时复发2 例)。另外,保留肝外胆管,不仅为后续的治疗提供更多选择方式,也减少了相应并发症的发生。切除肝外胆管行胆肠吻合术后再行肝动脉化疗栓塞或射频治疗,容易引起缺血性胆管炎或胆管坏死,引发肝脓肿[26-27],从而限制HCC伴BDTT术后复发的治疗手段。
本文的“q”形胆管切开取栓衍生于胆总管结石切开取石术。胆总管切开取石是治疗肝内外胆管结石最基本的手段[28-30],纵行切开胆管,然后使用胆道镜等器械取出结石。该术式给了我们灵感:延长胆管纵行切口,使BDTT完整暴露,再环形横断胆管,即可完整切除肝外BDTT。如何在术中取出B4型BDTT,目前尚无共识。Yamamoto等[18]报道了一种保留肝外胆管BDTT取栓方式—剥离技术。但这项技术也存在一些缺陷:⑴通过左右肝管的断端无法完全显露BDTT,取栓存在一定的盲目性;⑵如果癌栓侵犯肝外胆管,容易术后癌栓残留;⑶通过左右肝管断端锐性分离癌栓与胆管壁,不符合无瘤原则;⑷该方法不容易判断是否有癌栓残留;⑸该术式繁琐,需要阻断健侧肝管及胆总管下端。与剥离技术相比较,本文中的“q”形胆管切开取栓方法的优势:⑴完整显露BDTT,可一体化切除肿瘤及癌栓。且术中取栓过程不挤压肿瘤,更加符合无瘤原则;⑵充分显露胆总管,直视下可以更好的确认有无癌栓残留或侵犯胆管壁。如有癌栓侵犯胆管壁,术中可决定切除肝外胆管;⑶合并BDTT患者胆总管明显扩张,术后整形缝合胆管断端和胆总管壁,不容易发生胆管狭窄。
总之,“q”形胆总管切开取栓方法能够充分显露肝外胆管,取尽癌栓,是一种安全、有效、且符合无瘤原则的取栓方法。
[1]Qin LX,Tang ZY.Hepatocellular carcinoma with obstructive jaundice:diagnosis,treatment and prognosis[J].World J Gastroenterol,2003,9(3):385-391.doi:10.3748/wjg.v9.i3.385.
[2]Zeng H,Xu LB,Wen JM,et al.Hepatocellular carcinoma with bile duct tumor thrombus:a clinicopathological analysis of factors predictive of recurrence and outcome after surgery[J].Medicine (Baltimore),2015,94(1):e364.doi:10.1097/MD.0000000000000364.
[3]Meng KW,Dong M,Zhang WG,et al.Clinical characteristics and surgical prognosis of hepatocellular carcinoma with bile duct invasion[J].Gastroenterol Res Pract,2014,2014:604971.doi:10.1155/2014/604971.
[4]Navadgi S,Chang CC,Bartlett A,et al.Systematic review and meta-analysis of outcomes after liver resection in patients with hepatocellular carcinoma (HCC) with and without bile duct thrombus[J].HPB (Oxford),2016,18(4):312-316.doi:10.1016/j.hpb.2015.12.003.
[5]Pang YB,Zhong JH,Luo XL,et al.Clinicopathological characteristics and liver stem cell marker expression in hepatocellular carcinoma involving bile duct tumor thrombi[J].Tumour Biol,2016,37(5):5879-5884.doi:10.1007/s13277-015-4446-3.
[6]Zhang B,Zhang B,Zhang Z,et al.42,573 cases of hepatectomy in China:a multicenter retrospective investigation[J].Sci China Life Sci,2018,61(6):660-670.doi:10.1007/s11427-017-9259-9.
[7]Lin Z,Han M,Zhou Z.Prognosis for patients with hepatocellular carcinoma (HCC) with bile duct tumor thrombus (BDTT) after surgical treatment[J].Biosci Trends,2019,13(1):77-85.doi:10.5582/bst.2018.01234.
[8]Wang C,Yang Y,Sun D,et al.Prognosis of hepatocellular carcinoma patients with bile duct tumor thrombus after hepatic resection or liver transplantation in Asian populations:a metaanalysis[J].PLOS One,2017,12 (5):e0176827.doi:10.1371/journal.pone.0176827.
[9]Funamizu N,Mishima K,Ozaki T,et al.Pure laparoscopic right hepatectomy for hepatocellular carcinoma with bile duct tumor thrombus (with video)[J].Ann Surg Oncol,2020,28(3):1511-1512.doi:10.1245/s10434-020-09019-y.
[10]Sun J,Wu J,Shi J,et al.Thrombus-first surgery for hepatocellular carcinoma with bile duct tumor thrombus[J].J Gastrointest Surg,2020,doi:10.1007/s11605-020-04813-1.[Online ahead of print]
[11]Wong TC,Cheung TT,Chok KS,et al.Outcomes of hepatectomy for hepatocellular carcinoma with bile duct tumour thrombus[J].HPB (Oxford),2015,17(5):401-408.doi:10.1111/hpb.12368.
[12]Orimo T,Kamiyama T,Yokoo H,et al.Hepatectomy for hepatocellular carcinoma with bile duct tumor thrombus,including cases with obstructive jaundice[J].Ann Surg Oncol,2016,23(8):2627-2634.doi:10.1245 /s10434-016- 5174-7.
[13]冯锦凯,陈振华,武宇轩,等.肝细胞癌伴胆管癌栓诊治进展[J].中国实用外科杂志,2020,40(10):1210-1213.doi:10.19538/j.cjps.issn1005-2208.2020.10.27.
Feng JK,Chen ZH,Wu YX,et al.Progress on diagnosis and treatment of hepatocellular carcinoma associated with bile duct tumor thrombus[J].Chinese Journal of Practical Surgery,2020,40(10):1210-1213.doi:10.19538/j.cjps.issn1005-2208.2020.10.27.
[14]Peng BG,Liang LJ,Li SQ,et al.Surgical treatment of hepatocellular carcinoma with bile duct tumor thrombi[J].World J Gastroenterol,2005,11(25):3966-3969.doi:10.3748/wjg.v 11.i25.3966.
[15]Kasai Y,Hatano E,Seo S,et al.Hepatocellular carcinoma with bile duct tumor thrombus:surgical outcomes and the prognostic impact of concomitant major vascular invasion[J].World J Surg,2015,39(6):1485-1493.doi:10.1007/s00268-015-2985-9.
[16]Moon DB,Hwang S,Wang HJ,et al.Surgical outcomes of hepatocellular carcinoma with bile duct tumor thrombus:a Korean multicenter study[J].World J Surg,2013,37(2):443-451.doi:10.1007/s00268-012-1845-0.
[17]Inoue T,Ohashi T,Nakade Y,et al.Diagnostic utility of digital cholangioscopy for dislodged bile duct tumor thrombus of hepatocellular carcinoma[J].Endoscopy,2017,49(S01):E33-E34.doi:10.1055/s-0042-121007.
[18]Yamamoto S,Hasegawa K,Inoue Y,et al.Bile duct preserving surgery for hepatocellular carcinoma with bile duct tumor thrombus[J].Ann Surg,2015,261(5):e123-e125.doi:10.1097/SLA.0000000000001209.
[19]Sasaki T,Takahara N,Kawaguchi Y,et al.Biliary tumor thrombus of hepatocellular carcinoma containing lipiodol mimicking a calcified bile duct stone[J].Endoscopy,2012,44(Suppl 2 UCTN):E250-E251.doi:10.1055/s-0032-1309761.
[20]王庆新,严以群,吴孟超.肝细胞性肝癌伴胆管癌栓的手术治疗[J].中华肝胆外科杂志,2009,15(5):385-386.doi:10.3760/cma.j.issn.1007-8118.2009.05.025.Wang QX,Yan YQ,Wu MC.Surgical treatment of hepatocellular carcinoma complicated with bile duct cancer embolus[J].Chinese Journal of Hepatobiliary Surgery,2009,15(5):385-386.doi:10.3760/cma.j.issn.1007-8118.2009.05.025.
[21]Kim DS,Kim BW,Hatano E,et al.Surgical outcomes of hepatocellular carcinoma with bile duct tumor thrombus:A Korea-Japan multicenter study[J].Ann Surg,2020,271(5):913-921.doi:10.1097/SLA.0000000000003014.
[22]Hu XG,Mao W,Hong SY,et al.Surgical treatment for hepatocellular carcinoma with bile duct invasion[J].Ann Surg Treat Res,2016,90(3):139-146.doi:10.4174/astr.2016.90.3.139.
[23]Xu LB,Liu C.Hepatocellular carcinoma with bile duct tumor thrombus:extrahepatic bile duct preserving or not?[J].Ann Surg,2017,266(6):e62-63.doi:10.1097/SLA.0000000000001476.
[24]Shiomi M,Kamiya J,Najino M,et al.Hepatocellular carcinoma with biliary tumor thrombi:aggressive operative approach after appropriate preoperative management[J].Surgery,2001,129(6):692-698.doi:10.1067/msy.2001.113889.
[25]Wang HJ,Kim JH,Kim JH,et al.Hepatocellular carcinoma with tumor thrombi in the bile duct[J].Hepatogastroenterology,1999,46(28):2495-2499.
[26]Woo S,Chung JW,Hur S,et al.Liver abscess after transarterial chemoembolization in patients with bilioenteric anastomosis:frequency and risk factors[J].AJR Am J Roentgenol,2013,200(6):1370-1377.doi:10.2214/AJR.12.9630.
[27]Hoffmann R,Rempp H,Schmidt D,et al.Prolonged antibiotic prophylaxis in patients with bilioenteric anastomosis undergoing percutaneous radiofrequency ablation[J].J Vasc Interv Radiol,2012,23(4):545-551.doi:10.1016/j.jvir.2011.12.025.
[28]卢绮萍.肝胆管结石病外科治疗的历史与现状[J].中华消化外科杂志,2015,14(4):265-267.doi:10.3760/cma.j.issn.1673-9752.2015.04.002.
Lu QP.History and current status of surgical treatment for hepatolithiasis.[J].Chinese Journal of Digestive Surgery,2015,14(4):265-267.doi:10.3760/cma.j.issn.1673-9752.2015.04.002.
[29]何小东,刘乔飞.肝胆管结石病的诊断与治疗[J].中华消化外科杂志,2015,14(4):275-279.doi:10.3760/cma.j.issn.1673-9752.2015.04.004.
He XD,Liu QF.Diagnosis and treatment of hepatolithiasis[J].Chinese Journal of Digestive Surgery,2015,14(4):275-279.doi:10.3760/cma.j.issn.1673-9752.2015.04.004.
[30]尹飞飞,孙世波.肝外伴肝内胆管结石的微创治疗现状与进展[J].中国普通外科杂志,2014,23(8):1117-1120.doi:10.7659/j.issn.1005-6947.2014.08.021.
Yin FF,Sun SB.Minimally invasive treatment of concomitant extraand intrahepatic bile duct stones:current status and progress[J].Chinese Journal of General Surgery,2014,23(8):1117-1120.doi:10.7659/j.issn.1005-6947.2014.08.021.
